Legionnaires’ disease is a serious type of pneumonia you get when Legionella bacteria infect your lungs. Symptoms include high fever, cough, diarrhea and confusion. You can get Legionnaires’ disease from water or cooling systems in large buildings, like hospitals or hotels. Legionnaires’ disease can be life-threatening.
Legionnaires’ (LEE-juh-nares) disease is a type of pneumonia (lung infection) you get from breathing in Legionella bacteria. It can affect your lungs, brain and gut (gastrointestinal tract). Legionella also causes Pontiac fever, a less serious illness with flu-like symptoms. Legionnaires’ disease can be life-threatening.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
You get Legionnaires’ disease when Legionella infects your lungs. Most people with Legionnaires’ disease who are hospitalized have fever and cough but may also have other pulmonary symptoms such as diarrhea and confusion.
Most people don’t get Legionnaires’ disease, even if they’ve been around Legionella bacteria. But some people are more likely to get sick with a Legionella infection than others. You have an increased risk of getting Legionnaires’ disease if you:
Up to 18,000 people are hospitalized with Legionnaires’ disease each year in the U.S. It’s more common between June and October.
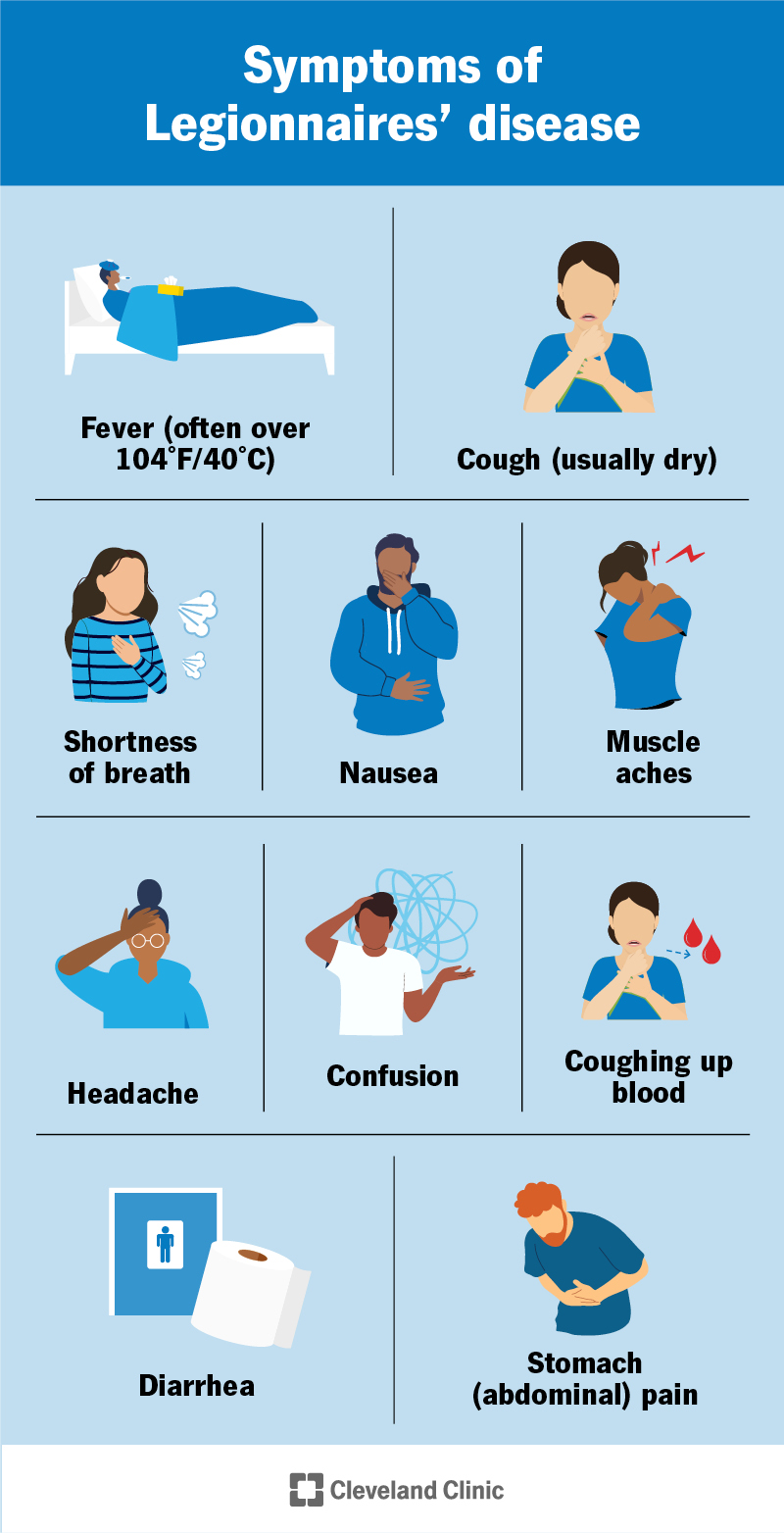
Legionnaires’ disease causes pneumonia-like symptoms that start two to 14 days after exposure to Legionella. You may also have neurological (brain) and gastrointestinal (gut) symptoms.
Symptoms of Legionnaires’ disease include:
Legionella bacteria causes Legionnaires’ disease. While there are at least 60 species of Legionella, Legionnaires’ disease is most often caused by Legionella pneumophila. You get Legionnaires’ disease when Legionella infects your lungs.
Legionella is found naturally in lakes, streams and soil, but it can also contaminate drinking water and air systems, especially in large buildings. You can breathe small droplets of water directly into your lungs, or water in your mouth can get into your lungs accidentally — for instance, if it goes “down the wrong pipe” (aspiration).
You can get Legionnaires’ disease by breathing in mist (aerosolized water) contaminated with bacteria or from getting contaminated water in your lungs (aspirating).
Outbreaks of Legionnaires’ disease have been described in hotels, hospitals, long-term care facilities or cruise ships, but most cases are random.
You can get Legionnaire’s disease from:
No, Legionnaires’ disease isn’t contagious. You can’t get it from another person.
Urine (pee) and sputum (mucus or phlegm) tests are the most common ways to diagnose Legionnaires’ disease. Your healthcare provider will also get pictures of the inside of your chest with an X-ray or CT scan.
Your healthcare provider will perform a physical exam and ask you about your health and travel history.
Tests to look for signs of Legionella bacteria and imaging are done to diagnose Legionnaires’ disease. These include:
The only way to know if you have an infection with Legionella is to be diagnosed by a healthcare professional. Legionnaires’ disease has symptoms of pneumonia, plus diarrhea and mental changes, like confusion.
Legionnaires’ disease is treated with antibiotics. You may get antibiotics through your veins (IV) or in a pill that you swallow. If you’re having trouble breathing, your provider may give you treatments to help you get enough oxygen. You’ll probably have to stay in the hospital while you’re treated.
Antibiotics used to treat Legionnaires’ disease include:
You may also receive extra oxygen through a tube in your nose or a mask. In serious cases, you may need to have a machine breathe for you until you can do it on your own again (mechanical ventilation).
Building managers can reduce the risk of Legionnaires’ disease by maintaining and properly disinfecting water and ventilation systems.
You can reduce your risk at home by making sure shower heads, faucets, hot tubs and humidifiers are properly cleaned. Don’t use plain water in place of windshield wiper fluid in your car.
Legionnaires’ disease can make you very sick, and you’ll probably need to be treated in the hospital. Fortunately, it can be treated with antibiotics.
After you go home from the hospital, you may still need to take medications to make sure the infection goes away completely.
For several months afterwards, you may still have:
Talk to your healthcare provider if you have concerns about ongoing symptoms.
Legionnaires’ disease can have life-threatening complications that affect your organs or muscles. They include:
Legionnaires’ disease is very serious, but most people survive. If treated, lung infections with Legionella are fatal about 5% to 10% of the time. If not treated, Legionnaires’ disease is fatal 30% to 80% of the time.
If you have symptoms of Legionnaires’ disease, contact your healthcare provider right away. If there’s an outbreak of Legionnaires’ disease in a building where you’ve worked or stayed, ask your provider what precautions you should take.
If you have a high fever, are struggling to breathe, are coughing up blood or have any neurological symptoms (like balance or speech problems or confusion), go to your nearest ER.
A note from Cleveland Clinic
Legionnaires’ disease is treatable but can be life-threatening. If you think you have Legionnaires’ disease or have stayed in an area with an outbreak, contact your healthcare provider right away.
Last reviewed by a Cleveland Clinic medical professional on 07/27/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy