A leadless pacemaker is a one-piece device a provider implants into your heart by way of a vein. Unlike with traditional pacemakers, you don’t need a separate battery under your skin or leads that go to your heart. Signals from a leadless pacemaker keep your heart beating normally.
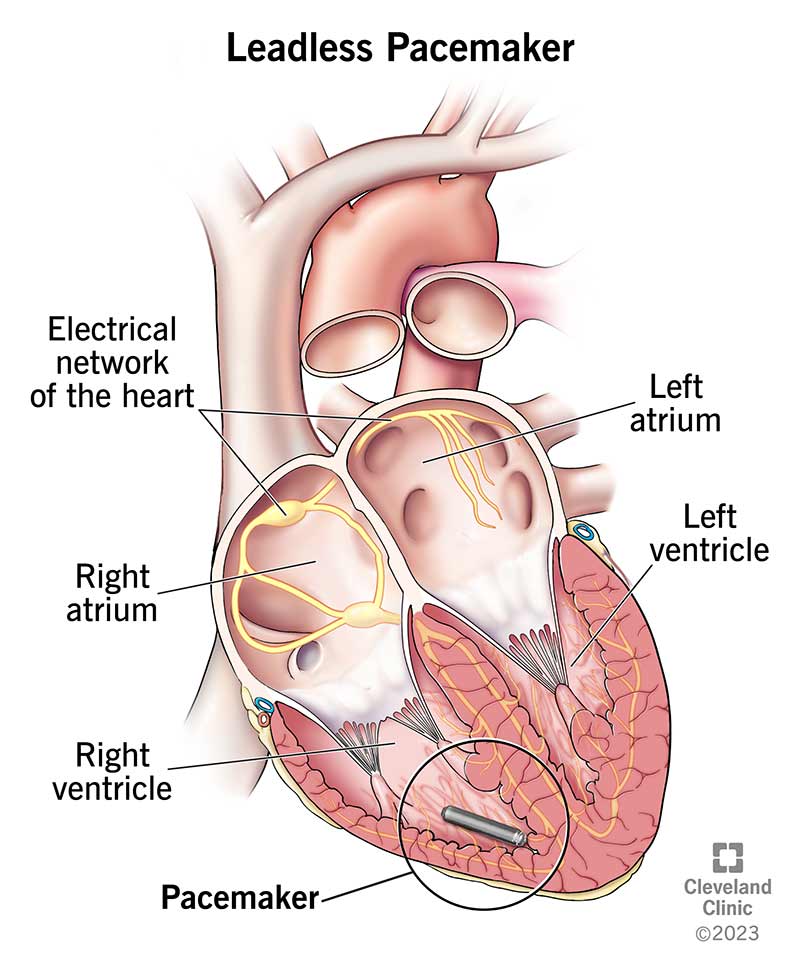
A leadless pacemaker is a small, one-piece device that a healthcare provider inserts into your heart to prevent slow heart rates. All the parts of a leadless pacemaker are inside one device. There’s no separate battery. And it doesn’t need leads (wires) because the whole device sits in your heart’s right ventricle (heart chamber).
Leadless pacemakers are about 1 to 1.5 inches (3 to 4 centimeters) long. The device looks like a small metal cylinder. It’s smaller than an AAA battery.
A healthcare provider programs and customizes your device to send small electrical impulses to your heart muscle when it needs it. A leadless pacemaker can sense your heart’s own electrical signals. It can provide additional electrical impulses when your natural ones aren’t frequent enough.
Pacemakers help people who have bradyarrhythmias, or slow heart rates. These are slow heart rhythms that may occur as a result of disease in your heart’s conduction system.
A provider may implant a leadless pacemaker when people have:
Some people aren’t candidates for a leadless pacemaker. Currently, the device is available only for people with certain medical conditions and a slow heart rate (bradycardia) who only need pacing in one heart chamber.
Your provider can tell you if you could receive a leadless pacemaker after reviewing your:
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Before receiving a leadless pacemaker, you’ll:
A healthcare provider will:
The procedure takes about 30 minutes to complete. However, this can vary from person to person based on the device and your anatomy.
After receiving a leadless pacemaker, you’ll need to:
Before your procedure, your healthcare provider will talk to you about leadless pacemaker pros and cons. They’ll help you decide on the device that’s best for you.
Benefits of a leadless pacemaker include:
Disadvantages of a leadless pacemaker include:
More serious but rare complications include the device moving out of place or internal bleeding, such as pericardial effusion or cardiac tamponade.
In studies, researchers found an implant success rate of 95% to 99%, with complication rates below 2%.
The battery in a leadless pacemaker lasts about 5 to 15 years. When the battery gets too low, a provider can turn off your old pacemaker and put in a new leadless pacemaker. The pacemaker itself may last 10 years. There’s enough room in your right ventricle for more than one pacemaker if they need to leave the old one there.
Yes, providers can remove leadless pacemakers.
Yes, leadless pacemakers are usually safe in an MRI under certain conditions. For example, there may be a limit on the strength of the magnet in the MRI machine that’s OK for you to use. A provider will check to ensure that you can have an MRI scan.
You can go back to everyday activities two weeks after receiving a leadless pacemaker.
A provider will check your leadless pacemaker:
They’ll want to make sure you’re healing well and your device is working without complications. They’ll also check your device’s battery charge at each visit.
Contact your provider if you:
You’ll need a leadless pacemaker for as long as you have the condition it treats.
Each year, more than 1 million people in the world get a pacemaker. Only about half of those who need a pacemaker are candidates for a leadless pacemaker. In the first four years after the U.S. Food and Drug Administration approved leadless pacemakers, more than 50,000 people received one.
A note from Cleveland Clinic
It can be unsettling to think about having a medical device in your body, but you aren’t alone. Millions of people across the globe have pacemakers. But leadless pacemakers aren’t a good solution for everyone; while a leadless pacemaker has advantages, a traditional pacemaker is a better option for some people. Talk with your provider about your questions and concerns.
Last reviewed by a Cleveland Clinic medical professional on 04/26/2023.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy