Coronary artery bypass grafting (CABG), also known as heart bypass surgery, is a procedure to restore blood flow to areas of your heart. Artery blockages can cut off blood flow, causing heart attacks or heart attack-like symptoms. CABG restores blood flow by using blood vessels from other parts of your body to create a detour around blockages.
Coronary artery bypass grafting is a surgery that restores blood flow to areas of your heart that aren’t getting enough blood. This surgery can improve your heart function and how you feel, especially when you’ve just had a heart attack or there’s an increased risk for you to have one in the near future.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Your heart works 24/7, supplying your entire body with blood. To do its job, your heart also needs blood flow, which it gets through a network of supply arteries that wrap around it. When tissues in your body aren’t getting enough blood flow, this causes a problem called ischemia (pronounced “iss-key-me-uh”).
The muscle cells in your heart are especially sensitive to ischemia, and when it's severe, those heart muscle cells will start to die. Coronary artery bypass grafting (abbreviated CABG and pronounced “cabbage”) treats ischemia by restoring blood flow to the affected heart muscle.
The condition that’s most likely to lead to CABG is coronary heart disease, a group of conditions that includes heart attack and coronary artery disease. Other conditions under coronary heart disease include angina pectoris, which is chest pain caused by ischemia in your heart, and silent myocardial ischemia, which is heart ischemia without any symptoms.
Conditions that fall under coronary heart disease usually involve a narrowing of the arteries in your heart because of a buildup of a fatty, wax-like residue called plaque. As plaque builds up on the inside of your heart's arteries, the arteries become stiffer and narrower. If an area of plaque breaks open, blood clots can form there and create blockages in those arteries. Those blockages cause ischemia in parts of your heart, which can lead to a heart attack.
The average age for people who have CABG surgery is around 66 years old. About 72% of the people who undergo it are men.
CABG surgery is very common, with about 200,000 such procedures happening every year.
CABG is major surgery, and people who have this done must first undergo a wide range of tests and other preparations.
Before you can undergo CABG, you will need to undergo several tests to see if it's safe for you to have this surgery and whether or not you need the surgery in the first place.
The potential tests include, but aren’t limited to, the following:
Part of preparing for CABG involves informing and educating you on what to expect and what you need to do before and after surgery to help you have the best possible outcome. Topics that you'll learn about include:
CABG is a complicated procedure that takes several hours to complete (the actual time needed depends on the specific type of CABG surgery, how many bypasses you need, and more). The following steps happen for most of these surgeries.
Like most major surgeries, the first step to this surgery is to put you into a state of deep sleep. This keeps you from feeling pain during the surgery. It also helps relax you for other steps in the preparation.
Because CABG involves work on your heart, it usually involves multiple types of life support. These include:
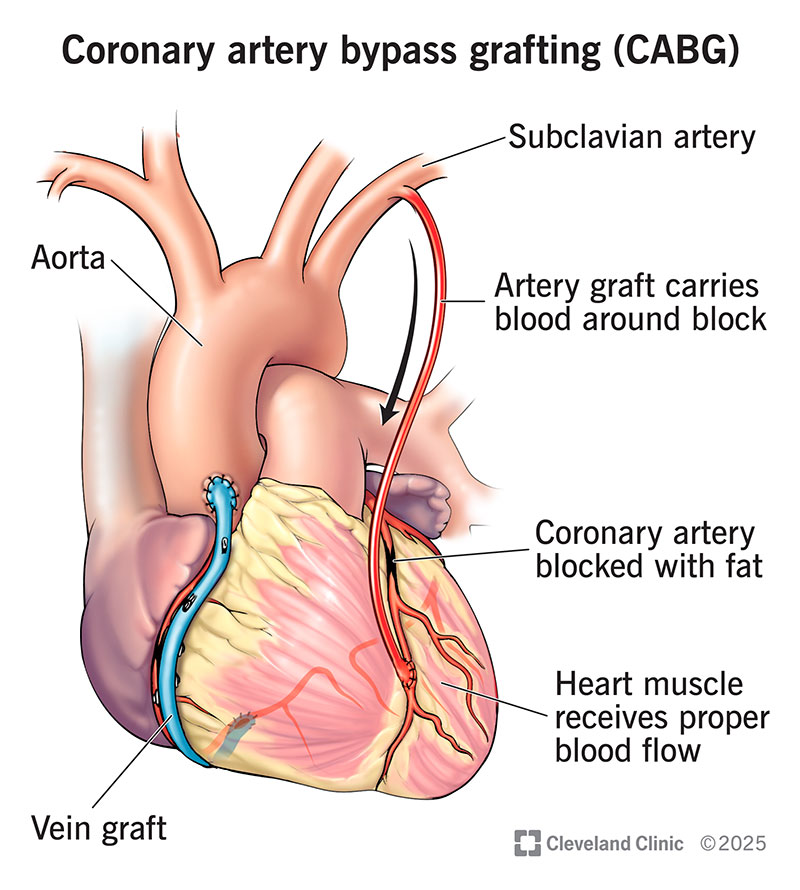
CABG involves creating a bypass for blood to use to reach blocked areas of your heart. A bypass is like a detour for your blood to use to get around an obstacle. Creating that bypass involves taking a blood vessel from somewhere else in your body, such as your leg, arm or chest, and using it to craft the detour around the blockage. In cases where there’s more than one blocked artery, multiple bypasses may be necessary. These are double (2), triple (3) and quadruple (4) bypasses.
To reach your heart to perform the surgery, a cardiothoracic surgeon will make an incision in the center of your chest. They’ll also split your breastbone (sternum) down the middle, then spread and lift your rib cage to make it easier to access your heart.
Once they reach your heart, the surgeon will take the harvested blood vessel and craft the bypass. The upper end (beginning) of the bypass attaches to your aorta, the large artery that carries blood out of your heart and to the rest of your body, just after it exits your heart. The lower end (ending) of the bypass will attach to the blocked artery just past the blockage.
Once the bypass is in place, the surgeon can restart your heart (if they stopped it) and get your blood flowing again. They’ll then lower your rib cage back into place and wire it together so it can heal. They’ll then close the incision in your chest with staples and sutures (stitches).
While CABG tends to use the same techniques in most people, there are instances where different techniques are better for your particular needs. The variations of this surgery include:
After surgery, people who undergo CABG go to the hospital’s intensive care unit (some hospitals use different terms like critical care unit). Staying in the intensive care unit (ICU) is necessary because ICU staff have specialized training and experience that is better suited for people with specialized needs like those who’ve just undergone CABG.
Once a person is stable and a doctor feels they’re ready, they can transfer to a regular medical-surgical room in the hospital for the remainder of their stay. The average hospital stay for CABG is between 8 and 12 days (longer for people who had CABG because of a heart attack, shorter for people who had stable ischemic heart disease or similar problems).
After leaving the hospital, most people who have CABG will also complete a cardiac rehabilitation program. Often called cardiac rehab, these programs help you recover and rebuild your strength after intensive cardiac procedures or events like heart attacks. Cardiac rehab programs include specially trained and highly qualified staff. They usually include nurses, exercise physiologists, nutritionists and dietitians, counselors and behavioral health specialists and doctors.
CABG has several advantages that make it a useful and common part of treating heart problems.
CABG is a major surgery, which means there are some potential risks and complications. While most of these risks and complications are avoidable or treatable, it’s still important to understand them. Possible risks include:
Most people who have CABG will need several weeks to fully recover from this procedure. During that time, your provider will likely have you avoiding any strenuous activities or situations that might put too much stress on your heart and incisions.
Your healthcare provider is the best person to tell you how long it will probably take you to recover and what you should expect. They’ll also tell you when you can start resuming your regular activities like work, exercising, driving, etc.
You should see your healthcare provider as recommended after your procedure. They'll schedule follow-up visits where they can check your heart function, remove any remaining stitches or staples, and make sure your wounds are healing well.
During your recovery, you should also follow your provider’s guidance regarding the following:
You should go to the hospital right away if you have any of the following:
A note from Cleveland Clinic
Coronary artery bypass grafting is a surgery that can make a big difference in how you feel and your overall length and quality of life. It's also a major procedure, and it’s normal to worry or feel anxious about having this surgery. Talking to your healthcare provider is important because they can provide you with information and resources that can help you better understand what’s happening. They can also guide you on what you can do to help yourself avoid complications and have the best possible outcome.
Last reviewed by a Cleveland Clinic medical professional on 01/11/2022.
Learn more about our editorial process.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy