Understanding this fastest growing joint replacement

When advanced osteoarthritis in the shoulder results in pain and loss of function, and nonsurgical treatments no longer help, joint replacement surgery may become an option.
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Advancements in implant design and more careful patient selection have improved outcomes and longevity of shoulder replacement in recent years. More than 70,000 of these surgeries are done annually, making shoulder replacements the fastest growing joint replacement.
Osteoarthritis is a common reason for shoulder replacement. But it’s not the only one. “We offer shoulder replacement to middle- and older-aged adults with chronic shoulder pain, mostly from arthritis or chronic rotator cuff problems,” says orthopaedic surgeon Vahid Entezari, MD.
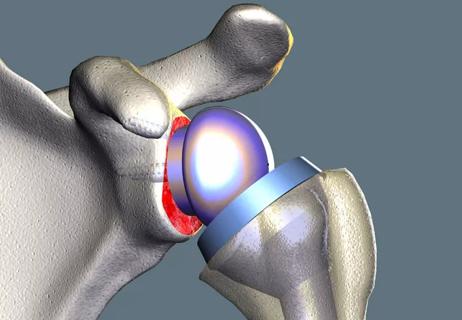
The shoulder is a ball and socket joint. A bony ball at the top of the upper arm bone (humerus) fits into a shallow socket (glenoid) in the shoulder blade (scapula). Four muscles that are called the rotator cuff surround the joint and provide stability and a wide range of motion.
The shoulder joint can develop osteoarthritis from overuse, trauma or an inflammatory process. The rotator cuff can also be damaged by a traumatic injury, but more often it weakens and tears over time as a function of aging.
Osteoarthritis is a degenerative condition commonly caused by the wearing down of cartilage, which is the shiny material covering the ends of the bones that allows for smooth movement. “Cartilage gets thinner and thinner, and you can get to the point where you have bone-on-bone arthritis,” says Dr. Entezari.
Chronic pain is generally felt in the upper arm and the front and back of the shoulder. It is aggravated by movement, especially overhead activities. There can also be a clicking and catching sensation. Stiffness develops in the advanced stage. “It gets difficult to raise your arm and reach around to your back” says Dr. Entezari.
Initially, osteoarthritis can be treated with nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy to improve range of motion. Corticosteroid injections often are effective, but they stop working as arthritis worsens. When these measures no longer help, joint replacement surgery can be considered.
Degenerative rotator cuff tears, which occur from wear and tear over time, are very common. They don’t always cause symptoms. When they do, the pain pattern is similar to osteoarthritis. However, people tend to have more weakness than stiffness.
Rotator cuff tears are initially treated with the same types of nonsurgical measures as osteoarthritis. If these fail in a young and active person who had an injury and the rotator cuff tear is not massive, usually surgery to repair the muscles is the first option.
“The goal is to save any rotator cuff that can be repaired,” says Dr. Entezari. But if the tear is too long-lasting, there is muscle loss, or it can’t be repaired, the person may be a candidate for an alternative to traditional (anatomic) shoulder replacement, called reverse shoulder replacement. People for whom previous repair attempts have failed also may have this surgery.
With the anatomic total shoulder replacement surgery, a two-part implant replaces the joint. The component that goes on the upper arm bone is a metal ball usually connected to a stem that is inserted down the humerus. The other component is a cup-shaped piece of plastic to replace the socket.
“This is called an anatomic shoulder replacement because the implant mimics the normal shoulder anatomy,” says Dr. Entezari. Patient satisfaction with this procedure is above 90%. The longevity of shoulder replacement has improved significantly. About 90% of people who’ve had this surgery for osteoarthritis still have their original implant after 15 years.
“We used to put long stem implants down in the humerus,” says Dr. Entezari. “With newer implant designs, we use shorter stems, and if the bone quality is good we can use stemless implants.” This makes surgery less invasive and preserves more bone.
The design of the socket side has also improved with use of more durable materials and implants that fit better.
A limitation of anatomic shoulder replacement is that you must have an intact rotator cuff. This is because the rotator cuff keeps the ball seated in the shallow socket at the shoulder joint. Other muscles around the shoulder move the joint.
People with weak or torn rotator cuffs can’t have an anatomic shoulder replacement. They may be able to have the reverse procedure.
Reverse shoulder replacement is similar to the anatomic version, except the positions of the two components of the implant are reversed. “We put the ball on the socket side and the socket on the ball side,” says Dr. Entezari. This solves the problem of not having rotator cuff muscles to keep the joint stable because the socket can be made deeper and the two parts of the implant are linked.
Reverse shoulder replacement is primarily done for people with a chronic rotator cuff tear who have developed arthritis. It may also be done for very severe arthritis that has led to significant bone loss, bone fractures that can’t be repaired, and when anatomic shoulder replacement needs to be revised.
With both shoulder replacement options, you will usually go home the day after surgery. Advancements in anesthesia have improved postsurgical pain control and reduced the need for pain medications.
By the second week, pain usually is diminished, and you will slowly gain the ability to move your shoulder. Four to six weeks after surgery you will do passive range-of-motion exercises. This will be followed by active range-of-motion and strengthening exercises.
Most people have good function after three months and continue to strengthen their shoulders. “By one year, most people stop thinking they have a shoulder replacement.”
Both procedures are very effective for pain relief. After the anatomic procedure, you should gain near-normal range of motion. With a reverse shoulder replacement, you will probably lose 10 to 20% of range of motion, especially in reaching your back.
This article originally appeared in Cleveland Clinic Arthritis Advisor.
Learn more about our editorial process.
An orthopaedic surgeon outlines the alternatives

Pain meds, toenail protectors and petrolatum jelly may spare you a trip to a podiatrist

An ice bath can ease sore muscles and decrease inflammation after a workout

Wrist flexor and extensor stretches are the best stretches for wrist pain

Simple exercises like tendon glides and finger lifts can have a big impact

They can last 10 to 15 years, but factors like age and activity level can impact their longevity

It’s a normal, common occurrence, but popping with pain or swelling may be a sign of an injury

Safe to wear for most people, compression socks promote better blood circulation in your legs

Your metabolism may torch 1,300 to 2,000 calories daily with no activity

A gentle touch in all the right places may help drain your sinuses