An asthma action plan is a personalized, step-by-step set of instructions for handling asthma attacks
Asthma attacks can be unpredictable and scary. But planning for them ahead of time can ensure that you get the help you need — fast.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Pulmonologist Rachel Taliercio, DO, explains what an asthma action plan is, why you need one and how to create it.
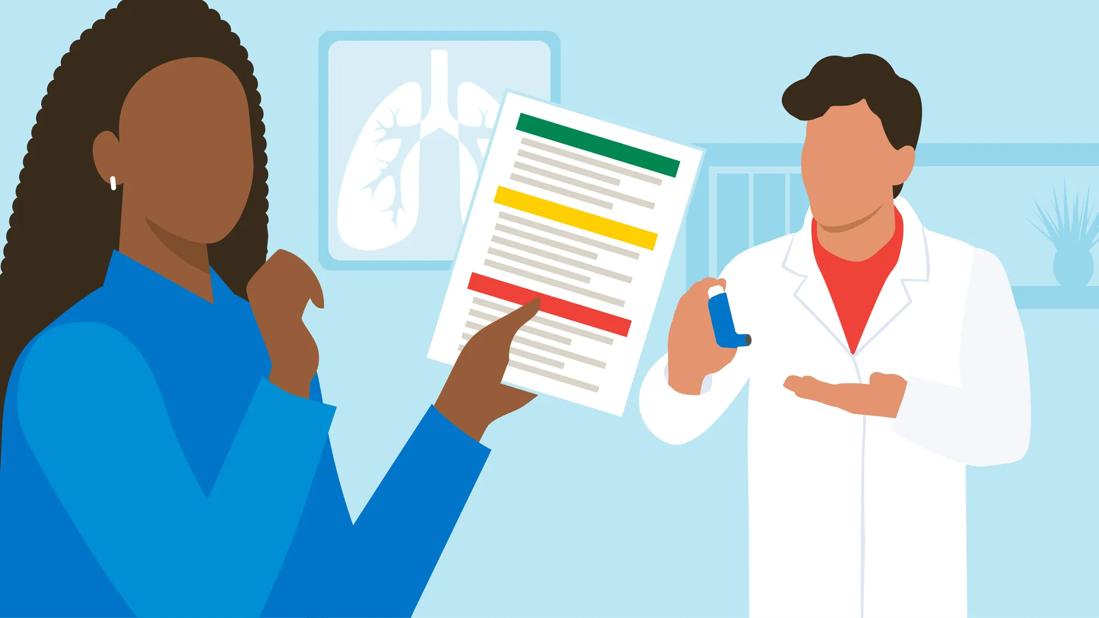
An asthma action plan is a personalized document that spells out the nature of your asthma, the meds you need and the actions to take during an attack. It’s broken down into three stages, so it’s clear what steps to use based on your symptoms. It takes the guesswork out of responding to an asthma attack, which can save time and help you stay calm.
“Having a plan in place isn’t just helpful when you get sick,” Dr. Taliercio explains. “It can also help you manage your asthma day-to-day. It’s equally useful for caregivers, physicians and emergency contacts. And if you’re a parent, it’s a crucial resource for childcare workers and teachers.”
An asthma action plan is built with the help of your provider and is broken into three different categories or zones. They’re color-coded to help readers figure out the steps they need to take to best help you.
| Your zone | What it means |
|---|---|
| Green | You’re doing well. |
| Yellow | You’re having an asthma attack. Call your provider. |
| Red | You’re having a major asthma attack. Call both your provider and 911 or emergency services. |
| Your zone | |
| Green | |
| What it means | |
| You’re doing well. | |
| Yellow | |
| What it means | |
| You’re having an asthma attack. Call your provider. | |
| Red | |
| What it means | |
| You’re having a major asthma attack. Call both your provider and 911 or emergency services. |

Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/a4c265f8-d67c-43ef-ae94-1ae2c6da0863/Asthma-Action-Plan-infographic-1304995012)
Each zone in your asthma action plan will have:
Advertisement
Dr. Taliercio says an asthma action plan should also have content that isn’t specific to the three zones, like:
An asthma action plan makes managing your condition easier and gives you peace of mind. But it’s also a useful tool to share with people who care for you. That includes your family, professional caregivers and emergency contacts.
If you’re drafting an asthma action plan for a child, share it with their school. That means their teachers, the school nurse and anyone responsible for their well-being, from carpool parents to coaches. Also, check to see if your child’s school or school district has policies around asthma medications and emergencies.
What if you have an asthma attack when you’re out and about? Dr. Taliercio recommends carrying a copy of the plan (along with a peak flow meter and any meds you need) with you. If you worry about losing the paper, wear a medical alert bracelet with a QR code on it. That way, first responders can access your plan with their phones.
Expect to update your asthma action plan with your provider during every office visit, in response to changing symptoms.
“An asthma action plan isn’t a one-size-fits-all document,” Dr. Taliercio points out. “It’s personalized to your needs. And those needs may shift. So, the plan’s not set in stone.”
Having an asthma action plan is great, but you also have to know how to follow it. Here are some tips to help you get comfortable using your plan:
Advertisement
“Having an asthma attack can be scary, but there’s power in preparation,” Dr. Taliercio reassures. So, don’t hesitate: Make an appointment to create (or update) your asthma action plan today.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement

Wearing a scarf, adjusting your outdoor activities and following your asthma treatment plan can help limit breathing problems

Adult-onset asthma has the same symptoms as childhood asthma, but tends to be more severe

Checking the weather, pollen counts and air quality can help you avoid asthma triggers

Stress can trigger and worsen asthma symptoms, like coughing and shortness of breath

Smoking, including secondhand smoke, can worsen your asthma triggers and damage your airways

Nighttime asthma attacks can be due to acid reflux, allergens and hormonal changes, but treatment can help prevent them

The effectiveness and safety of many of these options are unknown, so it’s best to stick to traditional care

Avoid triggers like dust, smoke and cold air to lessen your chances of coughing

Even small moments of time outdoors can help reduce stress, boost mood and restore a sense of calm

A correct prescription helps your eyes see clearly — but as natural changes occur, you may need stronger or different eyeglasses

Both are medical emergencies, but they are very distinct events with different causes