The world is getting warmer and fungi are evolving
Viruses are always finding new ways to change and adapt to their surroundings in an effort to infect people. This is how they’re able to reproduce. We see that happen every year with influenza and we’ve seen that happen with COVID-19 and its many variants. But what about fungi? Can they also evolve and survive in humans?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
HBO’s The Last of Us raised that question when it premiered. Based on a video game of the same name, The Last of Us presents a world ravaged by fungi that are able to adapt and infect humans at a rapid rate even though they couldn’t infect humans before.
While the game and show are entirely fiction, there’s some scientific concern involving new and emerging fungi that are infecting humans for the first time. And some fungi that have been around for a while are even becoming resistant to anti-fungal medications. That means some common fungal infections are becoming harder to treat.
Clinical microbiologist Anisha Misra, PhD, explains which fungi are now major areas of concern for ongoing research and how fungal infections work differently from others.
It helps to understand the science of how most infections evolve and spread from one person to the next. There are several kinds of infectious diseases caused by a variety of foreign bodies that include:
An infection can occur when one of these harmful organisms enters your body. Depending on the organism itself, they can enter your body in a variety of ways. And each has different effects.
Advertisement
For example, you can get infected with influenza by inhaling the virus through your nose or mouth. You can also catch the flu by touching a contaminated surface or a person who is infected and then touching your face, nose, eyes or mouth.
Giardiasis is another common illness, caused by the parasite Giardia, which can spread through contaminated water, food and other surfaces contaminated with trace amounts of feces. You develop this infection by swallowing the parasite.
And Creutzfeldt-Jakob Disease is part of a family of rare neurodegenerative brain disorders called transmissible spongiform encephalopathies (TSE). TSEs are caused by a buildup of prions in your brain. You can develop a specific variant of this infection, variant CJD, from eating beef from a cow that had bovine spongiform encephalopathy (BSE), better known as “mad cow disease.”
As you can see, the origin of every infection is different, but for the most part, they’re caused by harmful organisms that enter your body by being swallowed or inhaled. These infectious agents can also get into your body through an open cut, scrape, bite, scratch, sore or wound.
But outside sources aren’t the only way you can get infected. You can also develop what’s called a commensal infection. These infections occur when an imbalance or overgrowth of specific kinds of bacteria, yeast or fungal spores inside your body leads to illness. Examples of commensal infections include:
“We live with commensal organisms every day, and for the most part, they don’t tend to bother us at all,” says Dr. Misra. “But if a healthy human then develops a compromised immune system, that’s when we start to see infections. It’s because our immune system is not able to keep those microorganisms in check, so they’re allowed to proliferate and cause infections.”
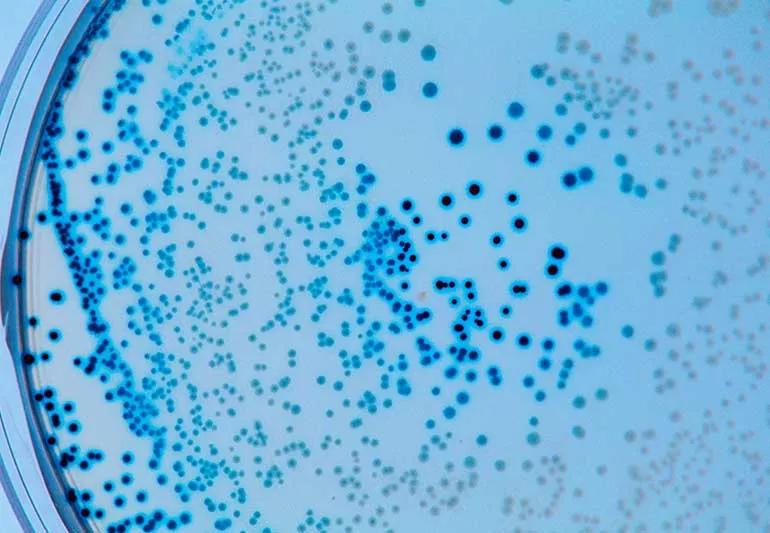
Fungi can be present as mushrooms, yeast, molds or a combination. All fungi are opportunistic in nature, meaning fungal spores are all around us (and inside of us) at all times — but they can cause illness if the right circumstances present themselves.
“Fungal spores are everywhere,” notes Dr. Misra. “With every breath we take, we’re taking in a significant amount of spores. But they’re not always causing infections.”
For people who are immunocompromised, fungal infections are particularly challenging and life-threatening because their weakened immune system allows for increased infections and rare infections to take root. Older populations are also more vulnerable to fungal infections.
Fungal infections are widely different in the way they look and feel and how they’re treated. Common fungal infections related to fungi include:
Advertisement
Studies show that fungal infections are actually responsible for 1.6 million deaths worldwide every year. That’s in line with deaths caused by tuberculosis and more than three times higher than deaths caused by malaria. Coupled with the fact that people are now living longer and we have more populations of people who are immunocompromised, fungal infections, in particular, have become a growing area of interest in research.
The reason for this is twofold:
Advertisement
“All of these things are bringing a more increased attention to fungal organisms,” says Dr. Misra.
In October 2022, the World Health Organization (WHO) made the first global effort to drive research and policy interventions around a list of 19 fungal pathogens that pose the greatest global threat or have the largest gaps in knowledge. Among those listed, four have been labeled as critical:
Advertisement
“Candida auris is a big one that was originally found in an ear canal in Japan, but since then, it’s shown up in various different institutions independently across three different continents,” says Dr. Misra.
The U.S. Centers for Disease Control and Prevention (CDC) has also listed this yeast as a priority because of its resistance to multiple antifungal medications. In 2022 alone, 17 states identified cases of C. auris for the first time. From 2020 to 2021, screened cases of C. auris tripled in the U.S. for a total of 4,041 infections.
“Because these fungal organisms have been able to adapt and cause infections within humans, they’ve become organisms of interest,” explains Dr. Misra.
In The Last of Us, a zombie apocalypse is caused by cordyceps — parasitic fungi that invade and take over specific, unique insects around the world before spreading their spores to others of that same species.
Cordyceps has been popularly referred to as “the zombie fungus” because of its ability to invade its host, cause behavioral changes and control its movement without ever directly impacting the brain.
“Studies have shown that cordyceps doesn’t actually affect the brain but it releases some type of chemical, toxin or protein that results in these behavioral changes,” says Dr. Misra. “There are some hypotheses that this fungus has more impact on the muscles than on any neural activity.”
There are more than 750 species of cordyceps and each one only affects a specific kind of insect in a specific region. But for anyone worried about whether cordyceps can infect humans, you can rest easy for the moment.
Cordyceps can’t yet infect humans, largely because cordyceps is not thermotolerant. Our high human body temperatures would kill off any spores that enter our bodies. In fact, some kinds of cordyceps have been used in traditional Chinese medicine for their potential health benefits.
But what if the world were to continue to get warmer? Could cordyceps adapt and jump from insects to humans? Could the fungus survive in humans?
“The Last of Us brings up a valid point: Cordyceps could eventually develop thermotolerance to infect individuals with a higher body temperature,” says Dr. Misra. “But the traits or features that allow this fungus to infect insects are very different than what it would take to infect a human being and cause the changes the show entertains us with.”
The Last of Us joins others in a long history of zombie myths rooted in scientific truth. If the world continues to heat up, fungi will continue to adapt. But just how fungi will continue to evolve and the ways they will affect us remain to be seen. That’s why ongoing research is needed more now than ever before.
“It took millions of years of coevolution in order for cordyceps to infect the particular species it targets,” adds Dr. Misra. “If cordyceps were to ever develop thermotolerance and infect us, it’s even possible that we could still be asymptomatic (have no symptoms).”
Because fungal infections are so varied, symptoms are widely different, too. For instance, if you have a fungal infection on your skin, you may experience itching, a rash or discolored and cracked nails. If you have a fungal infection in your lungs, you may develop a cough, fever, fatigue or shortness of breath.
Like with any infection, if you experience any signs or symptoms of illness, you should see a healthcare provider for treatment. If you’re given an antibiotic to treat the infection and the infection doesn’t go away, you may want to talk to your healthcare provider about antifungal treatment options.
“It’s important to use antifungals sparingly but also take them as prescribed,” advises Dr. Misra. “Some antifungal agents have mild side effects, but some can cause serious issues like liver and kidney damage, anaphylaxis (severe allergic reaction) and allergic skin reactions that can cause blisters and peeling skin.”
Another reason to use antifungal medications sparingly is to prevent fungal organisms from developing a resistance to the medications we have.
“We have seen a rise in antifungal resistance especially since fungicides are used in agriculture,” she adds. “We have a limited arsenal of antifungals and improper use or too frequent use can lead to fungal infections not responding to a once-effective medication.”

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement

Over-the-counter antifungal creams usually get the job done, but it’s important to keep it from spreading in the meantime

Some natural home remedies may offer relief, but they lack scientific evidence and won’t typically cure the condition

Chilblain-like skin lesions and rashes are mild (and rare) complications of many viral infections, not just COVID-19

Yes, but symptoms can be easy to miss

‘Walking pneumonia’ is milder and doesn’t always require medication — but it’s also highly contagious

From washing your hands and disinfecting surfaces to boosting your immune health, there are many ways to reduce your flu risk

Most can return to work or school when they’re symptom-free for 24 hours

Covering your mouth when you cough and staying home when you’re sick are a couple ways to help keep yourself and others COVID-free

Even small moments of time outdoors can help reduce stress, boost mood and restore a sense of calm

A correct prescription helps your eyes see clearly — but as natural changes occur, you may need stronger or different eyeglasses

Both are medical emergencies, but they are very distinct events with different causes