Tips to help your pain management specialist help you

When you’re in pain, getting through the day can be tough. So can finding the right solution for relief.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
There are many causes and types of pain, and everyone experiences it differently. A pain specialist can help develop a treatment plan for your unique situation. But they need your input.
Effective communication with your doctor is a key piece of the pain management puzzle.
“While most people think pain is all the same, there are actually several different types of pain,” explains pain management specialist Robert Bolash, MD. “Physicians who understand your challenges will have the best opportunity to find treatments directed toward each specific type of pain.”
Here’s how you can have more productive conversations about pain with your doctor.
In the most basic sense, pain is a biological process that protects you. When you get injured, your body produces chemicals that send pain messages to your spinal cord. The spinal cord delivers those messages to your brain, which process them and produces the sensation of pain. That’s called acute pain.
Chronic pain — which lasts for weeks, months or years — is a little more complicated. It often does not have an apparent purpose. It can hang around after an injury or surgery, or arise from a medical condition like arthritis or fibromyalgia. Over time, it can also result in changes to your nervous system that affect how you perceive pain.
Advertisement
“Unfortunately, chronic pain is not usually caused by one single problem — it’s rarely that simple,” Dr. Bolash says.
“Rather, chronic pain is often associated with a number of complex interactions that play different roles in the creation of pain signals from a site of injury to the brain.”
If you’re seeing a pain specialist for the first time, here’s what to bring to your appointment:
Unfortunately, there isn’t an effective measuring stick for pain, Dr. Bolash says. It can be challenging for doctors to gauge the level of pain people feel and whether treatments are effective.
To evaluate your pain, your doctor might ask you to rate your pain on a scale from 1 to 10, or request imaging studies such as an MRI or CAT scan. While these tools may be helpful, they often don’t tell the whole story. So your doctor will also rely heavily on your responses to questions about your pain, including:
This last point — describing what your pain feels like — doesn’t come naturally to most people, Dr. Bolash says. But being able to effectively communicate what you’re feeling can help your doctor better tailor treatments.
Here are some words that might help:
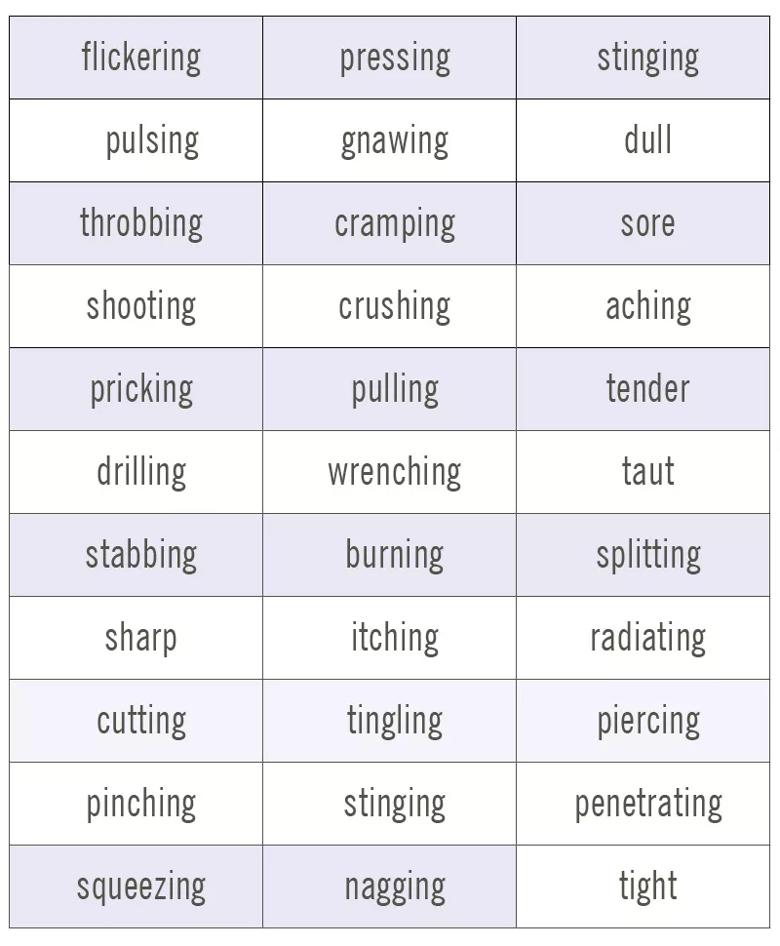
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/92efd470-df22-4887-b568-f56982ca3723/painWords-table1-800x970-1_jpg)
Dr. Bolash also recommends these tips for a productive appointment:
Advertisement
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement

Acute pain goes away with treatment, while chronic pain is long-lasting and can be complex to manage

Not all signals of physical pain actually make it to our brains — and you have some power over it

Find the right sleep position to tame your joint pain

Good pain or bad? Know the different kinds and when to seek help

Therapy helps pain sufferers get their sleep
In a major study, 93% of people saw a reprieve in pain

They put the kibosh on overzealous nerves

Gallstones can block bile in your biliary system and lead to pain and discomfort

Even small moments of time outdoors can help reduce stress, boost mood and restore a sense of calm

A correct prescription helps your eyes see clearly — but as natural changes occur, you may need stronger or different eyeglasses

Both are medical emergencies, but they are very distinct events with different causes