Having atrial fibrillation increases your risk of stroke — but blood thinners can help for many people

If you have atrial fibrillation (Afib) you may wonder whether blood thinners are right for you.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
After all, Afib is an irregular heart rhythm. Why would blood thinners need to be part of your management strategy?
Good question! And while there are other treatments for Afib, blood thinners are often an important part of the approach to keeping you healthy.
We talked with cardiologist Mandeep Bhargava, MD, about Afib and blood thinners and why they may be the key to lowering your risk of stroke.
Atrial fibrillation is a rapid and irregular rhythm of the upper chambers (atria) of the heart.
When you have Afib, the upper chambers of your heart are activated at a very fast rate — more than 250 to 350 beats per minute (bpm). For comparison, the expected resting heart rate for an adult is about 60 to 100 bpm.
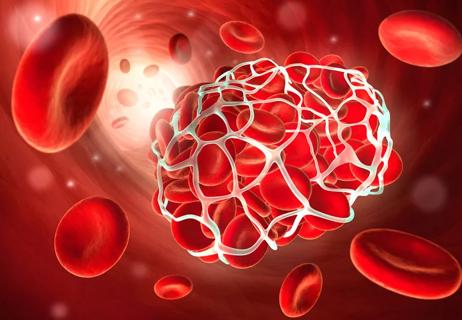
When you have Afib due to such rapid rates, your atria can’t squeeze as well as they should. That allows blood to pool and swirl in the left upper chamber, which puts you at increased risk for blood clots to form.
Those clots can then move to your brain and other critical organs (a process called embolization) and put that organ in danger. Your brain is the most commonly affected organ in this process. That’s why people with Afib are at increased risk of stroke.
Blood thinners (also called anticoagulants) reduce your risk of a stroke by making it less likely that clots will form.
Advertisement
“Blood clots can lead to stroke and also heart attacks and pulmonary embolism,” Dr. Bhargava reports. “Taking anticoagulants when indicated can help your body break down blood clots if they form — or prevent them from forming in the first place. In patients with atrial fibrillation, taking anticoagulants can lower your risk of stroke.”
Anticoagulant medications act by inhibiting the various clotting factors in your blood. That makes them useful in dissolving or preventing clots in relatively low-pressure chambers, like the left atrium (upper left chamber), which is where blood clots related to afib are most likely to form.
Common blood thinners for people with Afib include medications like:
If you have Afib, it doesn’t necessarily mean that blood thinners are always needed for you.
It’s a matter of weighing the risk of stroke being off anticoagulants versus the risk of bleeding on anticoagulants.
Healthcare providers use a measurement scale known as a CHA2DS2Vasc score to help determine your risk for a stroke.
Here’s how to find your CHA2DS2Vasc score:
Add up your score.
If you have Afib and you’re male and your CHA2DS2Vasc score is 2 or more, most guidelines recommend blood thinners. The same applies if you’re female and your CHA2DS2Vasc score is 3 or more.
Anticoagulation is also recommended if you have hypertrophic cardiomyopathy, hyperthyroidism and rheumatic heart disease-related atrial fibrillation despite the CHA2DS2Vasc score.
Advertisement
The CHA2DS2Vasc score is for people who don't have a history of excessive bleeding or a predisposition toward bleeding. People with a higher risk of bleeding can be assessed using the HAS-BLED score to help determine whether blood thinners are right for them.
“People who are more susceptible to bleeding may not be good candidates for blood thinners,” Dr. Bhargava clarifies. “If your blood is already less prone to forming clots and you take blood thinners, you’re at risk for excessive bleeding from even a minor injury.”
Talk with a healthcare provider to understand the risks and benefits of taking a blood thinner and whether it’s the right option to help manage your Afib.
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement

Opt for plant-based foods and consider limiting alcohol and caffeine

Making healthy lifestyle changes ahead of surgery can help you avoid AFib after

The short answer from a cardiovascular researcher

Knowing the facts can make all the difference

Bleeding is a risk and warrants taking care, but the reward of this lifesaving medication is great

The short answer from a cardiologist
Understand drug-food interactions

Track your blood sugar levels and pay attention to any symptoms, like feeling thirstier than normal

Even small moments of time outdoors can help reduce stress, boost mood and restore a sense of calm

A correct prescription helps your eyes see clearly — but as natural changes occur, you may need stronger or different eyeglasses

Both are medical emergencies, but they are very distinct events with different causes