It's about more than cervical cancer risk
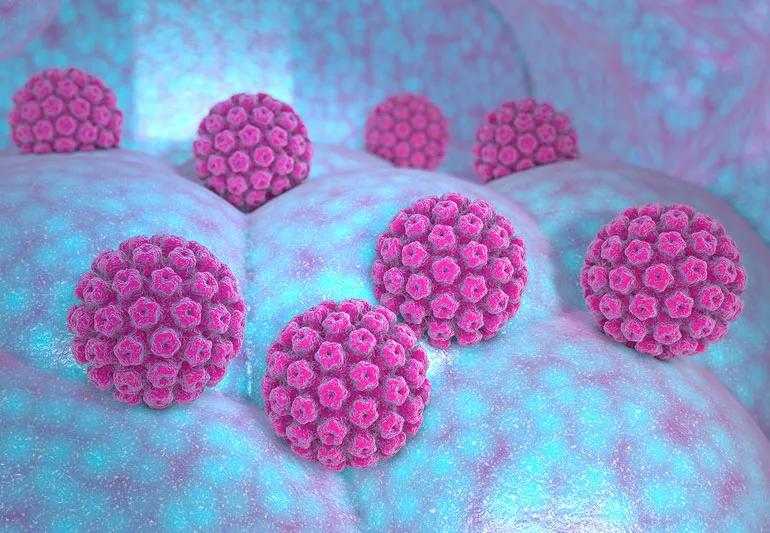
While human papilloma virus, or HPV, is a well-known cause of cervical cancer, there’s a lot more you should know about this common infection.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ob/Gyn Oluwatosin Goje, MD, shares seven things you probably didn’t know about HPV.
HPV is the most common sexually transmitted infection in the United States. According to the U.S. Centers for Disease Control and Prevention (CDC), about 79 million people are currently infected, and it’s estimated that almost everyone who’s sexually active will end up with at least one strain of HPV at some point.
In fact, only about a dozen strains of HPV are known to cause cancer, and two particular strains — HPV 16 and 18 — are responsible for about 70% of all cervical cancers. Some strains cause warts, but not cancer, and some strains cause no problems at all.
HPV is the leading cause of anal cancer and oropharyngeal cancer (cancer of the back of the throat). It’s also responsible for about half the cases of penile and vulvar cancer and about two thirds of vaginal cancer cases.
Actor Michael Douglas made headlines back in 2013 when he announced that he got throat cancer, not by drinking and smoking, but from HPV. In fact, white, nonsmoking men age 35 to 55 are most at risk for oral and oropharyngeal cancers caused by HPV; they’re four times more likely than women to develop these cancers.
Advertisement
Penile and anal cancer, while rare, are also caused by HPV.
Although there are ways to test for at least some kinds of HPV infections, the results don’t always tell you much about your cancer risk.
HPV infections often resolve on their own thanks to the body’s natural immune response, which means that you might test positive only to find out a few years later that you no longer have HPV at all. Testing is not a reliable way to screen for cancer or cancer risk.
Despite the limits of testing, it’s still a good idea for women to get a Pap test every few years (based on guidelines ) and for men and women to watch for other signs of HPV-related cancers so that you can catch any problems early. Here are some general recommendations.
It’s always a good idea to talk to your doctor about any changes you notice in these parts of your body.
Although HPV is widespread and in most cases doesn’t cause problems, there are ways to minimize your risks.
Advertisement
Knowing your risks and watching for changes in your body will go a long way toward limiting the chances that you will have problems with HPV-related cancers. Talk to your doctor if you have questions or suspect a problem.
Advertisement
Learn more about our editorial process.
Advertisement

The virus often clears up on its own within two years, but it can also linger and can cause further complications

Protecting yourself and others from a virus that causes cancer is the central focus

Chemo cold caps may help you keep more of your hair during therapy

Covering your mouth when you cough and staying home when you’re sick are a couple ways to help keep yourself and others COVID-free

There’s no safe way to find, handle, repair or remove asbestos yourself — it’s always a job for a professional

We don’t fully understand how cleanliness impacts immune system development, but we do know that preventing illness is important

Risks of this restrictive eating plan include digestive issues, heart disease and cancer

Breast cancer’s growth rate depends on its type, stage, grade and more

If you’re feeling short of breath, sleep can be tough — propping yourself up or sleeping on your side may help

If you fear the unknown or find yourself needing reassurance often, you may identify with this attachment style

If you’re looking to boost your gut health, it’s better to get fiber from whole foods