Advertisement
How the coronavirus causes acute respiratory distress syndrome
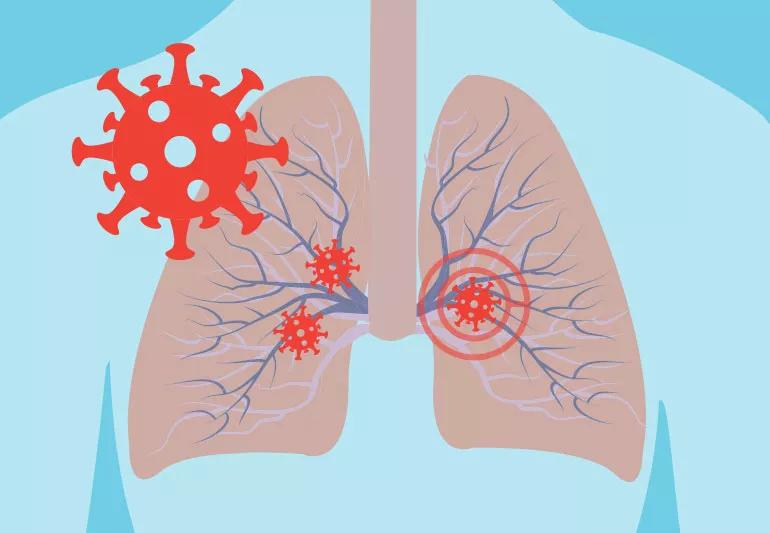
As the coronavirus (COVID-19) outbreak continues, we’re learning more about the disease, what it does to the body and the damage it can cause. But not sure you understand yet exactly what the virus can do to you?
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Although many people with COVID-19 have no symptoms or only mild symptoms, a subset of patients develop severe respiratory illness and may need to be admitted for intensive care.
In a new video, lung pathologist Sanjay Mukhopadhyay, MD, lays out in detail how the lungs are affected in these severe cases. The 15-minute video walks through how COVID-19 causes a “dangerous and potentially fatal” condition known as acute respiratory distress syndrome (ARDS) while providing stark images that underscore the severity of the damage that condition can cause to your lungs.
As Dr. Mukhopadhyay explains, Chinese researchers have linked COVID-19 to ARDS. Their study examined risk factors for 191 confirmed coronavirus patients who died while being treated in two hospitals in Wuhan, China.
The researchers found 50 of the 54 patients who died had developed ARDS while only nine of the 137 survivors had ARDS.
“It’s a really, really significant contribution to death in these patients,” says Dr. Mukhopadhyay.
If you have ARDS, you’ll have symptoms like sudden breathlessness, rapid breathing, dizziness, rapid heart rate and excessive sweating.
But the four main things doctors will look for are:
Advertisement
Most importantly, patients who are suffering from ARDS end up having damage to the walls of the air sacs in their lungs — the ones that help oxygen pass through into our red blood cells. That’s what doctors term diffuse alvelolar damage.
In a healthy lung, oxygen within these air sacs (alveolus) travels through to small blood vessels (capillaries). These tiny vessels, in turn, deliver the oxygen to your red blood cells.
“Nature has evolved in a way that the wall of alveolus is very, very thin in a normal person so oxygen can easily get from the air space in between to the red blood cell,” Dr. Mukhopadhyay explains.
The coronavirus damages both the wall and lining cells of the alveolus as well as the capillaries. The debris that accumulates because of all of that damage lines the wall of the alveolus the same way paint would cover a wall, Dr. Mukhopadhyay points out. The damage to capillaries also causes them to leak plasma proteins that add to the wall’s thickness.
“Eventually, the wall of the alveolus gets thicker than it should be,” he notes. “The thicker this wall gets, the harder it is to transfer oxygen, the more you feel short of breath, and the more and more you start moving towards severe illness and possibly death.”
The whole point, Dr. Mukhopadhyay stresses, is to emphasize what the coronavirus is capable of doing to a body, particularly high-risk patients who may be more vulnerable to infection. He hopes this will get people to take the current outbreak seriously.
“Please don’t dismiss this as ‘just another viral infection that will pass,'” he says. “Please take all the precautions that the CDC is outlining. Please protect yourself, your family, and others.”
Advertisement
Learn more about our editorial process.
Advertisement

Infection and inflammation can cause you to lose your voice and have other voice changes until you’re fully healed

A COVID-19 infection can bring on depression or anxiety months after physical symptoms go away

Just like the flu, COVID-19 continues to evolve every year with new and smarter variants

The latest omicron subvariants carry specific mutations that may allow the SARS-CoV-2 virus to be better at evading immune protection

Research shows the virus can affect your ability to get or maintain an erection

Getting vaccinated in October can help protect you against severe illness between November and March

Respiratory syncytial virus spreads easily through respiratory droplets spewed out by those who are infected

Face-touching is a common habit, but one that can be overcome, like by learning to recognize when you’re doing it and keeping your hands distracted

Not all ear infections need antibiotics — cold and warm compresses and changing up your sleep position can help

A glass of lemon water in the morning can help with digestion and boost vitamin C levels, and may even help get you into a better routine