How to know the difference
You know heartburn all too well. Maybe it happens after too much salsa. Or after any big meal. Or when you lie down.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Acid, partly digested food and other stomach contents creep up into your esophagus, causing the inside of your chest to burn like a jalapeño.
Most of the time it’s just acid reflux, or gastroesophageal reflux disease (GERD), which affects about 1 in 5 Americans. But for about 1 in 100,000 Americans per year, it’s actually a different condition, called achalasia.
Knowing which condition you have is important because acid reflux and achalasia are treated differently. If untreated (or treated incorrectly), you may continue to suffer with symptoms — and continued damage to your esophagus can become irreversible.
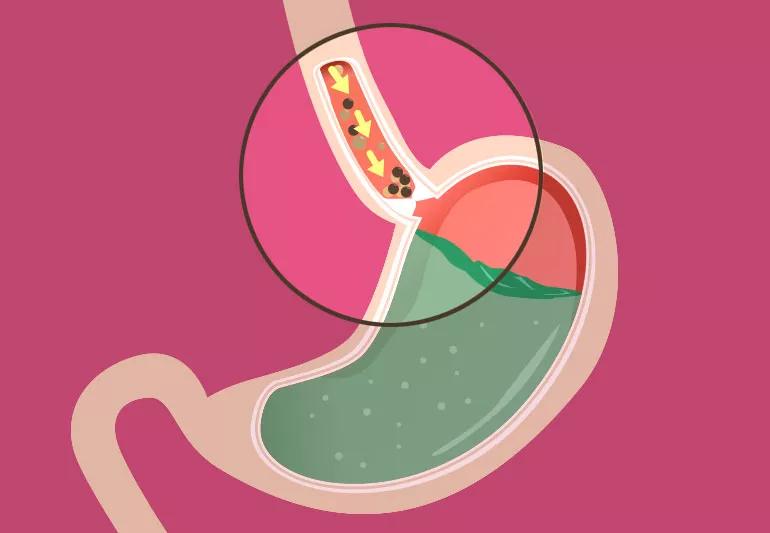
Both acid reflux and achalasia happen when the “door” from your esophagus to your stomach is broken. With acid reflux, the door doesn’t close when it should. With achalasia, the door doesn’t open when it should.
The door is called the lower esophageal sphincter. It’s a ring of muscle that should be squeezed shut most of the time. When you swallow, it should relax and open to let food into your stomach and then squeeze shut again.
“You may experience a small amount of acid reflux during this process,” says gastroenterologist Scott Gabbard, MD. “Up to one hour of acid reflux per day is actually considered normal.”
Advertisement
If you have achalasia, your lower esophageal sphincter doesn’t open. Whatever you swallow gets stuck at the bottom of your esophagus, which can cause heartburn, just like acid reflux.
It’s not clear what causes achalasia, but it has to do with the nerves that tell the sphincter when to open. Something causes those nerves to disappear, possibly an immune system response to a virus.
Because the conditions have similar symptoms, it’s not uncommon for people with achalasia to be treated for acid reflux — sometimes for years.
“If stomach contents come back up after you’ve swallowed them, most of the time it’s acid reflux,” says Siva Raja, MD, PhD, Surgical Director of the Center for Esophageal Diseases. “But if you have difficulty swallowing and feel like your food gets stuck in your esophagus, you should be tested to rule out conditions like achalasia and even esophageal cancer.”
A gastroenterologist may do an endoscopy to look in your esophagus or conduct a barium swallow or esophageal manometry to see how your esophagus is working.
Feeling like your food doesn’t go down to your stomach can be a sign of achalasia, but not always, says Dr. Gabbard. Acid reflux can cause ulcers at the bottom of your esophagus, which can cause food to get stuck, too.
If you have acid reflux, treatments usually involve:
If you have achalasia, acid reflux treatments typically won’t relieve your symptoms. Instead, your doctor may recommend:
Because achalasia is so rare, you may need to be referred to an experienced medical center for accurate diagnosis and treatment.
Advertisement
“I recommend different treatments for different patients,” says Dr. Gabbard. “The same treatment isn’t best for everyone.”
If you have heartburn and regurgitation once a week or less, try lifestyle changes and over-the-counter acid reflux medications first. If your symptoms don’t improve, see a doctor to be evaluated for achalasia or other conditions.
See a doctor sooner if you:
“Achalasia is a rare chronic disease,” says Dr. Raja. “Having regular follow-ups with an experienced specialist is important for long-term relief from symptoms and to ensure your esophagus is working as well as it can.”
Advertisement
Learn more about our editorial process.
Advertisement

What to know about dysphagia

It’s not an enema or bowel prep, and this colonic hydrotherapy can harm proper colon function

What’s on your plate, like lean chicken vs. fatty beef, may determine whether you deal with post-meal acid reflux

Family history can increase your risk of developing this autoimmune disorder — you may want to see a healthcare provider for screening

Choose foods that are easily broken down in your digestive system, like fruits and vegetables without skins or seeds

Focus on exercise, eating healthy and getting regular screenings to help lower your risk

A low-FODMAP diet or gluten-free diet could help you manage your symptoms, but only with professional guidance

A low-fat, high-fiber diet can help prevent gallbladder attacks and keep you pain-free

If you’re feeling short of breath, sleep can be tough — propping yourself up or sleeping on your side may help

If you fear the unknown or find yourself needing reassurance often, you may identify with this attachment style

If you’re looking to boost your gut health, it’s better to get fiber from whole foods