And how LBD differs from Alzheimer’s
Lewy body dementia (LBD) is the “other” dementia. It affects around 1.4 million Americans but doesn’t have the notoriety of Alzheimer’s disease. It’s flown under the radar of many medical professionals, and can be difficult to diagnose at an early stage, so patients are often misdiagnosed or wait several years to get the correct diagnosis.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
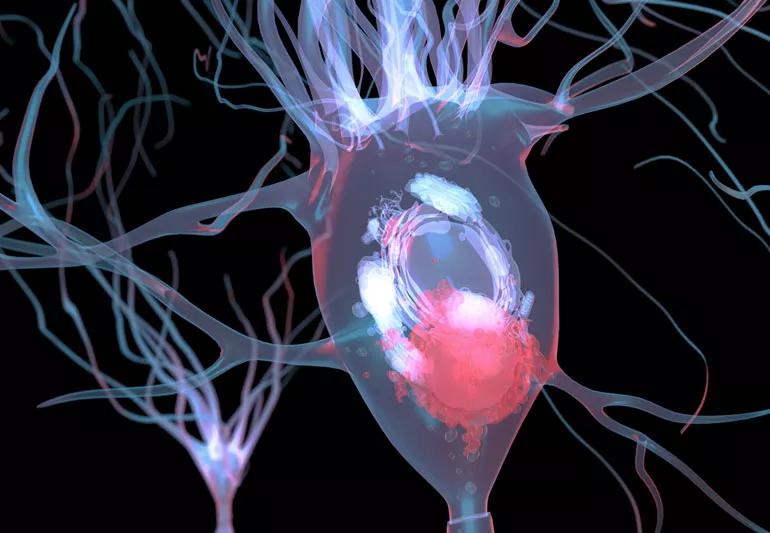
LBD can occur in individuals with Parkinson’s disease or have a similar onset of memory issues that one might see in Alzheimer’s disease. In both situations researchers see the characteristic “Lewy Bodies” in brain cells, thus it’s name.
The condition occurs when there are buildup of abnormal protein deposits in the brain cells that are responsible for behavior, thinking and movement. Neurologist James Leverenz, MD, explains the symptoms of LBD, how it’s diagnosed and what we can do to treat it.
“Dementia is the development of a change in thinking that affects day-to-day functioning,” says Dr. Leverenz. “While memory loss is the most well-known symptom of dementia, people with LBD don’t necessarily experience that early on. They often have more insight into the physical and mental changes they’re experiencing compared to people with Alzheimer’s disease.”
Like Alzheimer’s, LBD worsens over time. People with LBD commonly experience five symptoms:
1.) Mental slow-down
People find they get “off track” or distracted more easily. They recognize that they don’t process information as quickly as they once did. Multitasking becomes more challenging.
But who doesn’t have days when you can’t complete a sentence or you keep losing your glasses? Some trouble is normal with aging, but shouldn’t affect a person’s ability to perform their normal day to day activities
Advertisement
2.) Visual hallucinations
Patients with LBD may see things that aren’t there, like a dog or person. They may recognize that the objects don’t exist and usually aren’t frightened by them.
“It becomes problematic when people start believing their visual hallucinations are true,” says Dr. Leverenz. “If they call the police or can’t fall asleep because they’re scared, we may need to manage this symptom.”
If you are starting to see things that don’t exist, let a loved one or your doctor know.
3.) Parkinsonism
People often develop the same motor symptoms that occur with Parkinson’s disease. Talk to a doctor if you or a loved one start to experience:
4.) Fluctuations
“A family member, or affected person, may report that there are normal days but other times seems confused or sleepy,” says Dr. Leverenz. “Often the confused or sleep times clear up without any intervention.”
People with Alzheimer’s, on the other hand, tend to have confusion daily rather than sporadically. If you or a loved one experiences confusion or sleepy behavior a few times, it’s a good idea to check in with a provider.
5.) Sleep disorder
Patients often have a sleep disorder where they physically act out in their dreams. If their dream involves running, for example, their legs may be flailing about under the covers. These disorders can begin before any other symptoms — often years before — and are usually noticed by a bed partner.
“We can diagnose the sleep disorder with a sleep study. And there’s a high chance that a person with this disorder will develop LBD or Parkinson’s disease,” says Dr. Leverenz. “Often when someone comes in for an evaluation, and we ask about sleep disturbances, the bed partner says, ‘Oh, they’ve been doing that for years.’”
If your bed partner’s sleep antics wake you up, dial a doctor. Your partner may not have LBD, but they could have sleep apnea or another sleep disturbance worth treating — so you can both get your 40 winks.
Since some symptoms associated with LBD can occur with other conditions, it’s vital to seek care with a medical specialist who can provide a thorough evaluation and proper diagnosis (for example a neurologist, geriatric psychiatrist, or geriatrician). Neurologists will focus on managing problem-causing symptoms since there is no U.S. Food and Drug Administration (FDA)-approved medication that treats the Lewy body changes in the brain itself.
Advertisement
But medical specialists can often use medications and other interventions to:
“While we can’t cure LBD, we can provide effective symptom management that improves quality of life,” says Dr. Leverenz. “Finding a provider that has experience with Alzheimer’s and LBD ensures you or your loved one will receive specialized care. You won’t be offered medications that aren’t effective, or worse, cause unintended side effects.”
The National Institutes of Health and the pharmaceutical industry have funneled more resources into recognizing, diagnosing and treating individuals with LBD.
“Many of us are involved in these research studies and clinical trials. We’re hopeful that we’ll increase our understanding of the biology of the disease and how to treat individuals,” says Dr. Leverenz. “We’re just starting to see data coming out of those studies, and that’s very promising.”
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement

Physical activity can help preserve and improve your cognitive function and fend off dementia, stroke and other health concerns

When the familiar suddenly feels unfamiliar, it could be nothing — or something worth noting

Déjà vu is a fleeting, false memory — it can be harmless or a sign of something more

The ‘Six Pillars of Brain Health’ offers a game plan to maintain cognitive function

Studies show the medication may have a protective effect, but more research is needed

Decreasing estrogen levels can cause brain fog, but symptoms of dementia are different and more pronounced

Use a gentle, nonjudgmental tone, focus on prevention and reassure them that age-related memory issues can have a variety of causes

If you’re frequently dealing with short-term memory loss, confusion or issues around spatial awareness, you may need to see a neurologist

Even small moments of time outdoors can help reduce stress, boost mood and restore a sense of calm

A correct prescription helps your eyes see clearly — but as natural changes occur, you may need stronger or different eyeglasses

Both are medical emergencies, but they are very distinct events with different causes