They might not be fun, but colonoscopies are low-risk, high-reward procedures
Colorectal cancer is the third-most common cancer and the second-most common cause of cancer deaths.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Most people who get colon cancer are over 50. But in the last few decades, the rate of colon cancer has increased in younger adults. It can strike anyone, even otherwise healthy people with no family history of the disease.
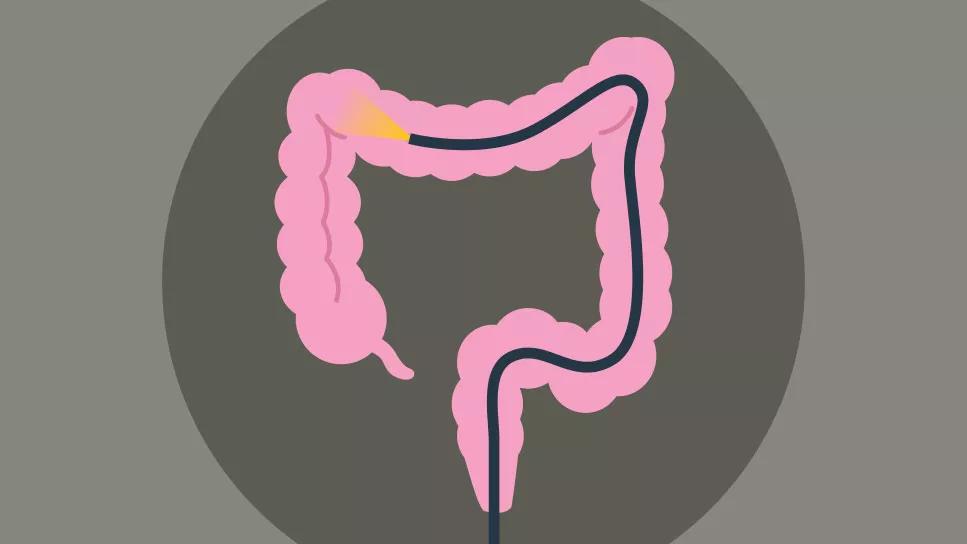
Colorectal cancer is common. It’s also preventable. “If you’ve got a colon, you’re at risk,” says colorectal surgeon Arielle Kanters, MD. But colonoscopies are the best tool to decrease your risk. Dr. Kanters helps us understand the risks and benefits of the procedure.
Colon cancer starts from growths called polyps that develop on the lining of the colon or rectum. Dr. Kanters says it’s common to have polyps. About 50% of us will have them show up during a colonoscopy at some point in our lives.
Not all polyps are dangerous, but certain types — mainly adenomatous polyps and sessile serrated polyps — can become cancerous. During a colonoscopy, providers spot and remove any polyps that look concerning. Removing the polyps (also known as a polypectomy) can significantly decrease your risk of developing colorectal cancer.
What makes this procedure so important? Part of it is just simple anatomy. You can’t identify polyps through a run-of-the-mill physical exam. In fact, you can’t feel them at all. And according to Dr. Kanters, neither pre-cancerous polyps nor early-stage, curable colon cancer causes symptoms.
Advertisement
“The point of screening colonoscopies is to get rid of polyps before they turn into cancer and become symptomatic,” Dr. Kanters explains.
The U.S. Preventive Services Task Force (USPSTF) recommends people between the ages of 45 and 75 get regular colorectal cancer screenings. If you have a family history of colon polyps or colon cancer, Dr. Kanters recommends talking with your provider. You might benefit from earlier screenings.
“How often you need to have a colonoscopy performed depends on a combination of factors, like what (if any) kinds of polyps we found on your previous colonoscopies and your personal and family cancer history,” she notes.
If you’ve read this far, it’s probably because you heard that your friend’s cousin’s neighbor’s dentist had a colonoscopy complication. It may be true! But they’re the exception Dr. Kanters says. Colonoscopies are extremely safe when performed by experienced specialists.
Of course, no medical procedure is entirely without risk. But — when it comes to screening colonoscopies — the risks are low. Here’s an example: Fewer than 1% of patients experience significant bleeding or a perforated bowel from a colonoscopy. By contrast, about 1 in every 21 people will develop colon cancer in their lifetime.
Colonoscopies are common procedures and complications, as mentioned, are rare. Dr. Kanters says that the risks associated with colonoscopies can increase based on your age, medications you take and other health concerns, but it can still be safely performed.
We’ve compiled a list of some potential side effects and complications. Spoiler alert: The list is short and the issues are mostly minor. It’s definitely nothing that should put you off the potentially lifesaving examination.
In order for the doctor to get a clear view of your colon, you have to be “cleaned out.” That means exactly what you think it means.
The prep process involves taking a powerful laxative and adjusting your diet in the days leading up to the procedure. Dr. Kanters says people are often wary of the amount and the taste of the laxative they have to drink to prepare their bowels for the exam. But those aspects of the bowel prep process have improved a lot in recent years.
“Cleansing formulas are more efficient than they used to be, so most people don’t have to drink nearly as much as they did in the past,” Dr. Kanters clarifies. “And the taste has improved as well.”
Of course, when you clear your bowels, you’re clearing more than just poop — you’re also losing fluid. In order to keep your electrolytes at a safe level, you need to replenish with plenty of clear liquids. If you don’t, you could end up dehydrated. Dr. Kanters also notes that adding those extra fluids will help the laxative be more effective.
Advertisement
“Sports drinks, clear broths, and teas and black coffee are great clear options for maintaining your electrolyte balance,” she says. Just steer clear of red, purple and other colorful flavors. They can stick around and look like blood.
It’s common to remove polyps or biopsy tissue during a colonoscopy, so a bit of blood in your poop (a little less than a teaspoon worth) is to be expected, according to Dr. Kanters. Bleeding only becomes a problem if it doesn’t stop, or the amount you’re losing is greater than a teaspoon. Dr. Kanters recommends calling the provider who performed your colonoscopy if you’re experiencing significant bleeding.
The risk of bleeding is higher for people who take blood thinners or have certain blood disorders, which is why it’s important to tell your provider about all of the medications you take and any conditions you have ahead of time.
Perforated bowel is a rare colonoscopy complication that tends to scare people. And understandably so! A perforation is a hole in the intestine, colon or rectum. Perforations can happen in many ways for many reasons and are most common in people with underlying medical conditions. In the context of a screening colonoscopy, a provider can perforate the bowel while manipulating the colonoscope, removing a polyp, cauterizing a polypectomy wound or — very rarely — while inflating the bowel. According to Dr. Kanters, small perforations usually get treated during the colonoscopy and rarely require hospitalization or surgical repair.
Advertisement
Now, when we say the risk of bowel perforation happening during your colonoscopy is low, we mean low. A review by the USPSTF suggests that for every 10,000 colonoscopies, there are four perforations.
In order to view the lining of your colon more easily, your provider will use air, carbon dioxide gas or water to slightly inflate it. As a result, Dr. Kanters says you might have some short-term gas or bloating after the procedure. That said, severe abdominal pain is unusual. If that were to happen,she recommends alerting the provider who performed your colonoscopy.
The kind of anesthetic used during your procedure is a topic you’ll discuss with your provider ahead of time. Some people receive general anesthesia, which actually puts you to sleep. Others get what’s called conscious sedation, or “twilight sleep.” With twilight sleep, the vast, vast majority of people are comfortable during the exam. In fact, Dr. Kanters says many people don’t even remember it afterward.
Like any other procedure performed under sedation, there’s a (low) risk of reacting poorly to anesthesia. That’s why there’s a trained team of providers monitoring you for signs of heart or breathing issues throughout your colonoscopy.
Advertisement
Just like any other medical procedure, there’s a risk of infection when you undergo a colonoscopy. In most cases, infections get treated with antibiotics.
You may have heard conflicting information about the value of colorectal cancer screening in people over 75 years of age. That’s because, Dr. Kanters says, it’s impacted by many factors, and should be determined on a case-by-case basis.
The conventional wisdom is that after age 75, the value of a colonoscopy diminishes enough that it isn’t necessarily worth doing. In fact, the USPSTF’s official guidance says, “Evidence indicates that the net benefit of screening all persons in this age group is small.”
So, if you’re over 75, should you get a colonoscopy or not? It’s up to you and your provider to decide. Dr. Kanters suggests that conversation with them cover these topics:
Reading a list of possible complications probably isn’t doing much to convince you that a colonoscopy is worth the discomfort. But it’s important to weigh the benefits against the risks.
When you do, it’s not even close.
Many providers consider colonoscopies “the gold standard” for a reason: They’re extremely effective. They can detect more than 95% of cancer cells and large precancerous polyps in the colon. From start to finish, the average colonoscopy takes about 15 minutes. Even figuring the bowel prep process into the equation, that’s a big return on a small investment of time and energy!
Colonoscopies may not be your idea of fun, but the time, preparation and (minimal) risk involved is worth it for most people between the ages of 45 and 75. Once you’re 75 years old, whether undergoing a colonoscopy is worthwhile depends on your health and your personal circumstances.
Whatever your situation, Dr. Kanters’ advice is simple: When in doubt, have a conversation with your provider. They can help you find the colon cancer prevention strategy that’ll work best for you.
Learn more about our editorial process.
Advertisement

Aim for soft, bland foods and extra hydration in the first 24 hours after the procedure

The caffeine and natural acids in coffee may trigger acid reflux, but there are ways to lessen the effects

Wait a few hours, then start with water or ice chips, graduating to clear liquids and then, soft, bland foods

Eating a healthy diet, reducing stress, and focusing on exercise and sleep can help keep your digestive system in top form

People with an inflamed esophagus may also have other conditions that cause a nagging, persistent cough

Your body naturally produces the protein that’s essential for breaking down and digesting food

Choose foods that are low in fiber and easy to chew and swallow

What, when and how much you eat are just a few factors that can impact nighttime gas levels

Wearing a scarf, adjusting your outdoor activities and following your asthma treatment plan can help limit breathing problems

Your diet in the weeks, days and hours ahead of your race can power you to the finish line

When someone guilt trips you, they’re using emotionally manipulative behavior to try to get you to act a certain way