About 35% of people with this autoimmune condition also develop uveitis
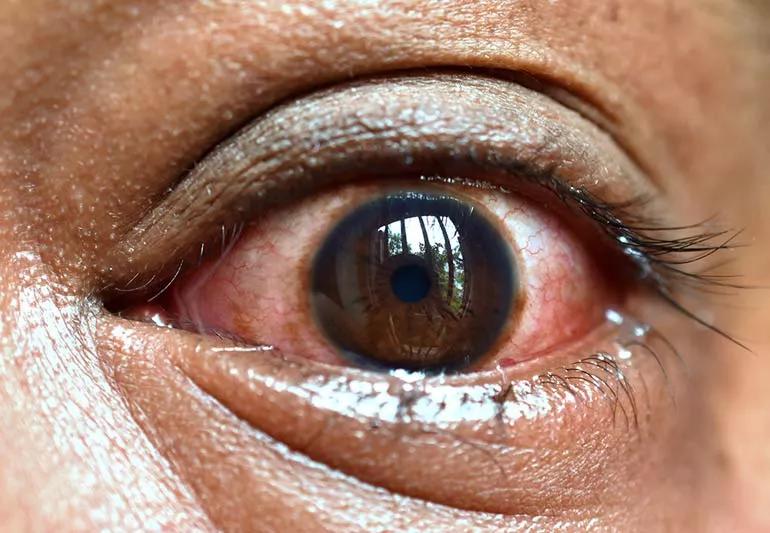
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/d026a8cc-c337-419b-8546-b96a129396aa/red-eye-pain-1321163552-770x533-1_jpg)
Closeup of irritated eye showing redness with blood vessels in eye.
Ankylosing spondylitis (AS) is a type of inflammatory arthritis that typically affects your lower back.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
While those who have AS may experience stiffness, fatigue and pain, the autoimmune condition can also cause eye inflammation known as uveitis.
Rheumatologist Ahmed Elghawy, DO, explains why you may experience eye problems and what treatments are available.
The short answer is: Doctors aren’t entirely sure.
“With autoimmune conditions like ankylosing spondylitis, your body is acting inappropriately against its own tissue,” explains Dr. Elghawy. “We think this is also the case when it comes to uveitis. There may have been some sort of pathogen that could have led to the body recognizing a self-antigen instead of the pathogen. The body makes the mistake of attacking itself.”
There may also be a link between a certain gene known as HLA-B27 that’s common in both ankylosing spondylitis and uveitis.
Between 25% to 35% of individuals with ankylosing spondylitis will go on to develop some sort of uveitis.
There are different types of uveitis:
Advertisement
“The longer the patient has ankylosing spondylitis, the more likely they are to develop uveitis,” says Dr. Elghawy.
Uveitis typically only affects one eye at a time; though, it’s possible to have symptoms in both eyes at once.
If you have uveitis, you may experience the following symptoms:
“In people who are older, uveitis increases the risk of developing cataracts or glaucoma or making those conditions worse,” says Dr. Elghawy.
If not treated, uveitis can harm your vision and could potentially lead to blindness.
“We recommend that those who have eye issues at all, especially who already carry a diagnosis of ankylosing spondylitis, that they let their doctor know immediately because it needs to be it needs to be addressed quickly,” emphasizes Dr. Elghawy.
Your doctor will not only treat uveitis, but will also treat your ankylosing spondylitis. In many cases, your rheumatologist may suggest you see an ophthalmologist, too.
Treatment options for uveitis may include anti-inflammatory eye drops or eye drops with corticosteroids.
Treatments options for AS can include:
Often, the biologic therapies used for ankylosing spondylitis also address uveitis.
“A common scenario would be a person who has low back pain and was treated with prescription or over-the-counter NSAIDs. They’re doing well, but later they develop eye issues, and then, that’s what kind of prompts us to start the biologic therapy,” explains Dr. Elghawy. “There are other individuals who are on biologic therapy who never go on to develop uveitis and that’s probably because they’re already being treated with the biologic therapy.”
And don’t overlook the importance of regular eye exams, says Dr. Elghawy.
“Sometimes, you may find evidence of uveitis during a typical eye exam, even before you have symptoms,” he adds. “So, it’s important if you do have evidence of uveitis, it’s treated properly to prevent the long-term consequences.”
Advertisement

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
Some diets are better than others, but it comes down to what works best for you
Pilates, stretching and hydrotherapy can support your spine and maintain a wide range of motion
Non-drug therapies like massage therapy and acupuncture can help manage pain, stiffness and fatigue
Doctors aren’t sure why, but the conditions are connected
Ease pain and stay active by keeping your spine in its proper position
Managing the chronic pain of this autoimmune condition is important
Act quickly by locating the object, gently removing the debris and flushing your eye
Pink eye tends to start in one eye before spreading to the other, while allergies usually affect both eyes at the same time
Prioritize your health by managing stress, strengthening your social connections and getting quality sleep
Bolsters, blankets, pillows and blocks can offer extra support, stability and comfort
Allergies, postnasal drip, asthma or reflux could be to blame for a cough that won’t quit