A timeline of what to know after delivering your baby

It’s been 40(ish) weeks. You’ve finally made it and you’re holding your new bundle of joy. What’s next? This is probably the biggest question swirling around in your head. It’s OK. Take a deep breath…
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Many things will change in the days, weeks and months following your pregnancy and delivery. You probably expected sheer exhaustion, frequent nighttime feedings and diaper change after diaper change. But one shift that you might not have anticipated is how your body reacts and heals after birth. Not only are you welcoming your little one into the world, but your body is also going through a major adjustment.
Midwife Elizabeth Beach, CNM, gives us a look at the next six weeks postpartum and what to expect as you recover.
Um, 18 years? But seriously. In total, it takes about six weeks to fully heal from giving birth. And while we have a good idea of how your body transitions during this time, everyone’s journey may be a little bit different. (Had a C-section? Your recovery will look different.)
Here’s what you can expect each week after a vaginal birth:
“Your postpartum recovery process actually starts right in the same room that you deliver in,” says Beach. “Your nurses will check your vitals and make sure you’re stable before you get transferred to the postpartum unit.”
From the day you give birth to the last day of the six-week period, your body will begin a healing transition.
Unless you choose to have a home birth, your first couple of days of healing after birth will be in the hospital. Most women stay between 24 and 48 hours after a vaginal delivery. “Once you’re in the postpartum unit, they’re still checking for your bleeding and vitals to make sure you’re all good,” explains Beach.
Advertisement
This can also be a good time to talk to a nurse or lactation specialist for advice if you choose to breastfeed your baby at home.
“Sometimes, this time in the hospital can last a little longer if you’re waiting on additional labs or testing,” Beach notes. This usually happens if your baby needs to get some extra tests done or has jaundice.
The first few days after delivery, you may still have contractions or cramping — these are sometimes called “afterpains.” While the pain is unpleasant (especially after just giving birth), it’s nothing to be alarmed about. This happens because your uterus is working hard to shrink down to its original size.
“A lot of people think that once the baby’s out and the placenta is out, it’s totally over,” says Beach. “But your body is still doing things to try to make sure that you stop bleeding. So your uterus is cramping, and you can feel it.”
This cramping should stop after a couple of days, but you can try putting a heating pad on your belly to make yourself more comfortable. If the pain becomes too much to handle, your healthcare provider should have sent you home with some over-the-counter pain relievers (usually ibuprofen or Tylenol®) to manage the pain as well.
The motto for the first two weeks after birth is “take it slow.” From feeding your baby to adjusting to how you don’t feel quite like you yet, it’s crucial to not rush your body into healing and to handle it with care. Depending on what your healthcare provider recommends, you’ll likely have a two- or three-week check-in to see how you’re doing post-delivery.
If you’ve decided to breastfeed, you probably have a lot on your mind. How do I know if they’re latched right? Is it right to be this sore — or is something wrong? But know that breastfeeding isn’t something you have to go at alone. You have the support of lactation consultants and your other breastfeeding moms to lean on.
“When you leave the hospital, chances are your milk has not come in yet,” says Beach. “It’s always a good idea to make a separate lactation visit within your first week because they can help with different feeding positions and any latching issues that might arise after coming home from the hospital.”
Your body will start producing milk about three to four days after giving birth — whether or not you’re choosing to breastfeed. If you do choose to breastfeed, you can expect to feel tender around the nipple area, but you can use nipple cream after every feeding to help with this.
Advertisement
Beach warns that if you’re having intense breast pain or soreness or notice a red area (warm to the touch) this could be a sign of mastitis. If you are experiencing this, be sure to talk to your Ob/Gyn provider.
If you’re not breastfeeding, your milk will dry up on its own. But you can speed up this process and feel more comfortable if you wear a tight sports bra (for as many hours as possible and as soon as you deliver) and avoid stimulating your nipples.
During the first couple of weeks, it’s normal to experience some vaginal bleeding and discharge — called lochia. This is a natural process your body goes through after birth. By the end of the second week, this should start to taper off (become less frequent).
“Your bleeding starts out like a really bad period, and it should progress like a period,” explains Beach. “So, it should always be getting a little lighter each day.”
The other thing you’ll notice, Beach points out, is a change in the color of your discharge. This reflects the three stages of lochia that your body is going through to get rid of blood, tissue and mucus.
“It might start out bright red. Then, it will progress to a brownish, darker red. And then, it might go to a light pink,” she continues. “It might get to a yellowish discharge color at some point. And those are all within the realm of normal.”
Advertisement
Your body just completed a huge feat, so it’s normal to feel a bit sore down there. A little bit of pain in the vaginal area can be expected. This will vary, depending on if you experienced a vaginal tear during delivery or if you had an episiotomy done.
You can relieve some of this pain or discomfort at home by:
During the first or second week of recovery, it’s important to not overexert yourself. Though you may be eager to shed those pregnancy pounds, the gym can wait! Try taking small, slow walks each day to stay active as the pain subsides. “You should start to feel better each day,” reassures Beach.
Another symptom you may experience within the first couple weeks after birth is a change in your bowel movements. During this time, you may have some difficulty having bowel movements due to the weakening of your pelvic muscles.
One minute you’re feeling fine. The next, you feel a rush of emotions hit you like a tidal wave. This is a common experience during the first couple of weeks after birth — often called the “baby blues.” It can be common for your moods to be on a bit of a roller coaster as your hormones are balancing out and you’re adjusting to a new routine with your baby.
Advertisement
But if these feelings of sadness or depression go beyond the first couple of weeks, you should talk to your healthcare provider to ensure you aren’t experiencing postpartum depression.
Mood swings are natural during the first two to four weeks after giving birth because your hormones are really changing, says Beach. “But if these mood swings persist and you’re starting to feel down or depressed — or like you don’t want to take care of yourself, your baby or your other kids — that’s something you should talk to your healthcare provider about.”
After about one week, you should have also lost most of your “delivery weight.” (We’re talking the weight of your baby, placenta and fluids here, NOT necessarily any extra pounds you may have gained.) Slowly, your body is transitioning back to how it was before you got pregnant, but this can look different for every person.
“The weight loss after pregnancy is really different for everybody,” says Beach. “You may have more of a visual change — your belly size will visibly reduce within the first couple of weeks. And you may come home from the hospital and look like you're still pregnant. So, it really depends.”
Three weeks means that essentially, you’re halfway there to a full post-partum recovery. Phew! By now, you’ve probably gotten more acquainted with your baby’s routine and are settling into breastfeeding or bottle feeding.
At this time, you should still be gentle with your body. The good news? You can slowly start going back to normal activities — but that half marathon may still have to wait though.
“At three weeks, you should start to feel like you’re starting to return to a more normal state,” says Beach. “Your body takes a while to repair completely after the process.”
After three weeks, you should start to feel your strength coming back. “You should feel comfortable taking a walk around the block,” says Beach. If you’re eager to get back on that treadmill, ask your healthcare provider about what exercises they recommend starting with. At the same time, your vagina is probably still in the process of healing, so your body may not be ready to return to sexual activity just yet.
A little bit is still OK, but there should be a noticeable decrease in your bleeding at this point. “Your bleeding should have stopped or at least slowed significantly,” states Beach.
Wow, does the time fly or what? Now, you’re six weeks in and you’ll have a chance to check in with your Ob/Gyn provider to see how you’ve been doing. By this point, you’re likely feeling mostly healed, and you’ll be asked about your physical and mental status.
Here are some things you should expect with your physical status at six weeks:
Before your six-week check-up, be sure to pay attention if your body is sending you any signals. Beach recommends seeing your healthcare provider if you’re experiencing any of the following:
Of course, we realize that an official “recovery” from giving birth might take six weeks, but your life will never look the same again. It’s important to spend those first weeks postpartum taking care of yourself, paying attention to your body’s signals and being patient with how you heal. And don’t hesitate to give your healthcare provider a call if you notice something is off or strange throughout your recovery.
Learn more about our editorial process.
Advertisement

Yes, new fathers can experience mood changes after bringing baby home

But if you’re worried, don’t hesitate to call your doctor or midwife

Heavy bleeding, pain and persistent sadness could be something more serious

Having sex after giving birth isn’t only about being medically ready

It’s normal to experience some changes
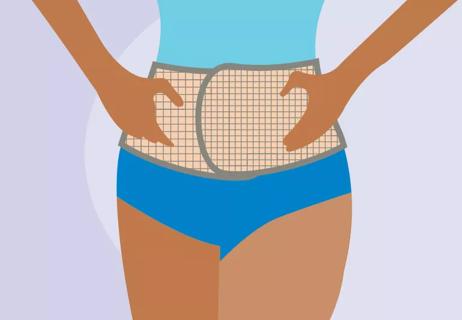
Belly wraps provide physical support after you give birth

Sad feelings and teariness that persist are a sign

Patience is the best solution

Start having sex about 72 hours before ovulation, then at least every other day during your fertile window

Attachment theory suggests that your earliest relationships shape connections throughout your life

It isn’t a recognized mental health disorder, but research shows that problematic social media use can negatively affect your mental health, self-esteem and sleep