Lifestyle changes, like a healthy diet and exercise, can help with fertility issues
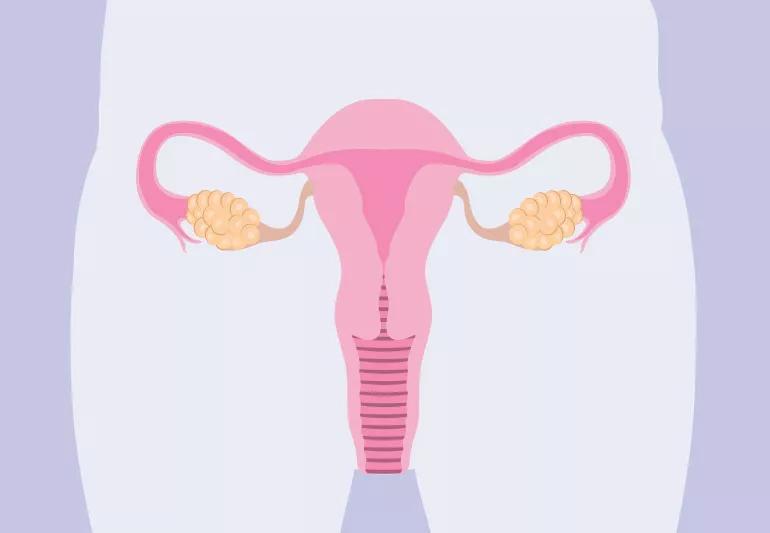
Image content: This image is available to view online.
View image online (https://assets.clevelandclinic.org/transform/3315e5fd-c025-4951-bcb9-5e07fb5b4ef4/pcos-uterusOvaries-1169701391-770x533-1_jpg)
PCOS and weight
The process of becoming pregnant begins with, and depends on, ovulation, when an egg is released from one of the ovaries to be available for fertilization.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Ovulation issues are the most common cause of infertility. They occur in about 20% of the 6.1 million women in the U.S. ages 16 to 44, who have difficulty getting or staying pregnant.
One of the most common conditions leading to ovulation problems is polycystic ovarian syndrome (PCOS).
And a diagnosis of PCOS can be a significant blow when you’re trying to start a family.
But can you get pregnant with PCOS?
Ob/Gyn Marjan Attaran, MD, fertility specialist Julierut Tantibhedhyangkul, MD, and bariatric surgeon Jesse Gutnick, MD, explain how PCOS impacts fertility and how to get pregnant with PCOS.
PCOS is one of the most common hormonal disorders and the leading cause of infertility in women ages 20 to 35.
A major feature of PCOS is hormone imbalance. Why PCOS happens isn’t clear.
Normally, hormones released by your pituitary gland in your brain control the ovulation process, regulating an egg’s growth and triggering your ovary when it’s time to release it. If the levels of these hormones change, your ovary may have difficulty developing and discharging a fully mature egg. Instead, unreleased eggs form tiny cysts inside of your ovary.
Ovulation issues most often involve having unpredictable menstrual bleeding patterns and/or intervals between periods that last longer than 35 days. To be diagnosed with PCOS, you must have at least two of these signs or symptoms:
Advertisement
“Not everyone who has polycystic ovaries have PCOS,” clarifies Dr. Tantibhedhyangkul. “In fact, about one-third have polycystic ovaries just because they’re young and have good eggs reserve, which means they have a lot of eggs inside their ovaries.”
Having obesity and PCOS are also typically related to one another.
“Those who have obesity have insulin resistance, which manifests itself differently around the body,” explains Dr. Gutnick. “In the pancreas, it shows up as diabetes. In the liver, it can develop into fatty liver disease. In the ovaries, PCOS. Patients can also develop PCOS at a young age, resulting in obesity later in life.”
The good news is that ovulation problems are often easier to treat than other types of infertility. Here are some things you can do to increase your chances of getting pregnant with PCOS.
When you lose weight, your insulin resistance decreases — improving PCOS conditions in one fell swoop. You can imagine what that does for your fertility.
Your care provider may also suggest bariatric surgery if your BMI is 40 and above. Women with BMIs between 35 and 40 can also benefit if they have associated conditions like diabetes, high blood pressure and sleep apnea.
As for the type of bariatric surgery that’s best, that depends on a comprehensive evaluation of your health and goals. Dr. Gutnick notes that for PCOS, it’s more about successful weight loss — propelled by healthy lifestyle changes — than procedure type.
“When someone has severe obesity, usually, it’s hard to lose weight. And if they can lose weight, it’s very difficult to keep it off,” he continues. “While we can help them with the lifestyle changes needed to lose weight and prescribe medications to boost results, some people's bodies have a ’set point’ that resists weight loss, even if they live a healthy lifestyle. That’s where bariatric surgery can help.”
If you’re trying to become pregnant, you want to ensure you eat healthy and get the proper nutrients.
Limit or avoid unhealthy fats, sugar and simple carbs, which are typically found in foods like baked goods, highly processed foods and fast foods.
Instead, you want to eat a diet rich in:
Advertisement
Your doctor may also suggest certain supplements or prenatal vitamins that may help with infertility like:
Your provider may order blood work for fasting glucose level and HgbA1C blood work, which shows your average blood sugars for the past three months. In some cases, they might recommend a test called a glucose tolerance test to screen for diabetes.
And while exercise and a healthy diet can help manage insulin levels, your doctor may also suggest metformin, a common medication used to treat Type 2 diabetes.
After taking oral drugs called antiestrogens (clomiphene citrate, brand name Clomid®) or aromatase inhibitors (letrozole, brand name Femara®), as many as 85% of people will be able to ovulate, and as many as 40% of those will conceive. The drugs adjust levels of the hormones that regulate ovulation.
Clomiphene citrate is approved by the U.S. Food and Drug Administration (FDA) for treatment of ovulation problems and is the drug that doctors normally use first to treat PCOS. It’s a pill taken for five days, beginning the second to fifth day after your period starts.
Advertisement
Common, mild side effects include hot flashes, mood swings, pelvic discomfort and tenderness in the breasts, shares Dr. Attaran. Taking clomiphene citrate brings a slightly increased chance (about 9%) of a multiple pregnancy (twins or more). Healthcare providers usually don’t prescribe the drug for longer than six months because its effectiveness drops off over time.
In the last decade, providers have been prescribing letrozole more often as an alternate treatment for PCOS, even though its FDA-approved use is as a breast cancer treatment. This is called “off-label,” which means it’s prescribed for a use other than its stated purpose.
“Some doctors opt for letrozole for their PCOS patients because it appears to be as effective as clomiphene citrate, but with fewer side effects and less risk of multiple pregnancies,” explains Dr. Attaran.
While a 2005 study suggests that letrozole may increase the risk of birth defects, follow-up research has not shown this to be the case.
If you have PCOS and are unable to become pregnant after taking either drug, you may still have success with more advanced infertility treatments. These PCOS fertility treatments include:
Advertisement
While it can be scary when you’re dealing with PCOS and trying to have a child, the outlook is bright. By working with a healthcare provider, you can explore what lifestyle changes and medications might work best for you.

Sign up for our Health Essentials emails for expert guidance on nutrition, fitness, sleep, skin care and more.
Learn more about our editorial process.
Advertisement
Hormonal imbalances and insulin resistance can cause weight to accumulate around your midsection
Diet won’t cure polycystic ovary syndrome, but healthy eating can help you feel your best
The supplement may help with weight management and blood sugar levels
PCOS can cause skin problems, but birth control pills, hormonal medications and topicals can help
The common hormonal condition is linked to insulin resistance, which can cause weight gain
While this hormonal condition can be hereditary, there are other risk factors to also consider
How these lifestyle changes may help restore insulin sensitivity
These over-the-counter kits are 99% effective at identifying when you’re most fertile each month
Although it could be used as a moisturizer, this new trend is not recommended
Communicating clear limits helps protect your time, energy and emotional well-being
High cholesterol can be genetic, but testing and treatment can lower your heart disease risk