Here’s how (and why) to ask your doctor about treatment goals, second opinions, clinical trials and more

It’s natural to have lots of questions after receiving a cancer diagnosis. But it’s also understandable if, in the midst of such major news, you can’t even figure out where to start.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
We turned to oncologist Suneel Kamath, MD, for some insight.
“Oncologists try to be as informative as they can,” Dr. Kamath says, “but it’s good to be proactive and ask as many questions as possible.”
When you’re diagnosed with cancer, your oncologist will tell you information, like:
You’ll want to dig deeper into all that information. But what else should you ask about? Dr. Kamath shares seven questions to ask your oncologist after you’ve been diagnosed with cancer.
First things first: Dr. Kamath says people are often too nervous or afraid to ask about getting a second opinion because they don’t want to offend their doctor. But when you’re first diagnosed, getting a second opinion is critical. It helps make sure your diagnosis and treatment plans are correct.
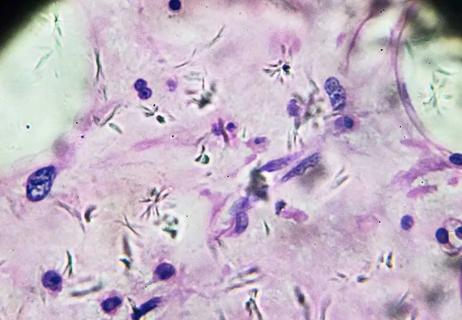
“A second opinion provides a second review of your pathology slides and pathology report, which is the original pathologist’s description of the findings that led to your diagnosis,” Dr. Kamath explains. “This is especially crucial if your diagnosis came from a smaller hospital, which often only has general pathologists and oncologists on staff.”
Advertisement
Large, academic cancer centers have various oncology and pathology subspecialists on staff. These doctors, who specialize in specific types of cancer, have likely diagnosed and treated more people with your type of cancer than a general pathologist or oncologist.
There’s another reason to seek a second opinion, too: Doctors are only human. A second set of eyes can only help.
“Not every doctor can know everything about every condition,” Dr. Kamath points out. “The field of oncology has exploded, and it’s very difficult to keep up with all the latest knowledge.”
Try not to worry about upsetting your doctor by asking for a second opinion. They’re used to it and even expect it — and they know it will bring you peace of mind.
It’s important to define the goal of your treatment upfront, at the very beginning of your cancer journey, so you understand what to expect.
Depending on the type and stage of cancer, your goal may be to:
“You might not be willing to put up with six months of side effects if your disease is likely to come back within a year,” Dr. Kamath says. “But you might tolerate a lot more side effects if you learn that your treatment is likely to get rid of your cancer entirely.”
Clinical trials test for ways to prevent, treat and diagnose cancer, while also managing your symptoms and possible side effects. And there are clinical trials available for every stage of cancer.
But Dr. Kamath notes that there’s a lot of misinformation and misunderstanding about this topic. Many people hesitate to ask their oncologist about clinical trials because they fear they’ll be used as pharmaceutical companies’ guinea pigs.
“In reality, people with cancer who participate in clinical trials generally do better than those who do not,” he says. “They’re getting tomorrow’s breakthrough therapy today.”
It’s important to know that any drug that makes it to phase III clinical trials has already been studied extensively. And that no one gets placebos or sugar pills alone in oncology clinical trials.
“All participants get at least the current gold-standard treatment, and some will also get the novel therapy that’s being studied,” Dr. Kamath explains. “So, if your oncologist offers you a clinical trial to participate in, be prepared with a list of questions about benefits, risks, costs and other treatment choices.”
Many types of cancer and cancer treatments can affect fertility, so if you think you may want to have biological children in the future, it’s important to ask your oncologist about your fertility options. And it’s important to do so before your treatment begins.
Advertisement
“Always raise the question prior to cancer treatment,” Dr. Kamath urges. “You might think fertility preservation will delay your treatment, and there are times when that’s true. But for many people, it doesn’t have to.”
So, what fertility questions should you ask? If you hope to conceive in the future, ask questions like:
If you’re a parent or guardian whose child has cancer, these same questions still apply. Childhood cancer treatment may affect their future fertility, so it’s important to get answers as early as possible.
It’s never easy to learn that you have cancer, whether you’ve been newly diagnosed or your cancer has come back. And you may not know where to turn for support.
“When you’re navigating cancer treatment, it’s very normal to feel sad and scared, and even to develop depression,” Dr. Kamath says. “Your oncologist can help you find the support you need.”
They can point you toward cancer support groups and other resources that can help you deal with your feelings around your diagnosis. They can also help connect you with mental health services, like a therapist who specializes in working with people with cancer.
Advertisement
When you’re dealing with a diagnosis, the last thing you want to think about is the fees associated with procedures, lab tests, surgery and medications. But cancer treatments can be costly, so ask your oncologist what to expect.
“It’s important to have a frank discussion about finances,” Dr. Kamath urges. “Out-of-pocket expenses like copays, medications and even parking can all really add up.”
If your doctor doesn’t know the answer, ask to talk to a social worker or financial counselor. They may be able to suggest financial assistance programs or other resources that can help.
“Financial toxicity from cancer care is real and common,” he acknowledges. “No one should feel ashamed or embarrassed to ask for help.”
Sometimes, cancer outsmarts the existing treatments. In these cases, conversations about death are difficult and emotional — but they’re also necessary.
“You and your oncologist should have an honest discussion about your best option,” Dr. Kamath says. “This doesn’t mean giving up. It means changing your focus from treating the cancer at all costs to focusing on your comfort and quality of life.”
Your oncologist can recommend services like hospice, which can help facilitate comfortable, peaceful end-of-life care, and individual providers like end-of-life doulas, who can help guide you through your grief. This is also the time to talk to your loved ones, including children, about what comes next — and your oncologist can help you find the right resources for that, too.
Advertisement
“If your doctor doesn’t raise these topics, speak up and ask,” Dr. Kamath advises. “These options can help you understand the process and spend more time at home with loved ones.”
Learn more about our editorial process.
Advertisement

Prioritize protein and fresh produce, but be extra careful to avoid bacteria that could cause foodborne illnesses

Rates of early-onset breast, colorectal and GI cancers are increasing, but preventive care and a healthy lifestyle can help reduce your risk

The side effects of cancer and treatment can impact desire, sexual function and intimacy, but there are ways you can keep the flame going

Decisions you make regarding smoking, alcohol use, meal choices and exercise can make a big difference

Taming fear and reclaiming your future after treatment
Carcinomas are the most common and affect skin and organs

7 healthy eating tips to help reduce your risk of some of the most common types of cancer

Research on the controversial issue is mixed, but there are safety precautions you can take

Wearing a scarf, adjusting your outdoor activities and following your asthma treatment plan can help limit breathing problems

Your diet in the weeks, days and hours ahead of your race can power you to the finish line

When someone guilt trips you, they’re using emotionally manipulative behavior to try to get you to act a certain way