Advertisement
Hospitals are taking extra precautions to keep patients safe

With the global COVID-19 pandemic at the center of public attention, it can be easy to forget that all kinds of other medical emergencies, like heart attacks and strokes, are still happening every day. But they are. (Every 40 seconds, someone in the U.S. has a heart attack, according to CDC data.)
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
Yet doctors worry that some people who need emergency medical care for illnesses not related to COVID-19 aren’t seeking it because they’re afraid of being exposed to coronavirus at the hospital.
According to studies, some hospitals have seen the number of patients showing up to their emergency departments drop – especially during the early days of the pandemic.
Some of that was to be expected, says Bradford Borden, MD, FACEP, Chairman of the Emergency Services Institute. “Not everyone is venturing out and doing all the activities they normally do,” he explains, pointing to a decline in emergency department visits for broken bones, accidents and traumas.
But it’s also worrisome. “The number of heart attack patients we’re seeing went down, but we know heart attacks aren’t going away,” he says.
For heart attacks and other medical emergencies, quick treatment can be the difference between life and death. So people should not avoid emergency care when they need it, Dr. Borden says.
Emergency departments are open and prepared to care for patients as safely as possible during the pandemic.
Health systems are taking many steps to keep their patients and health care workers safe during the COVID-19 crisis. Every hospital might do things a little differently, but they’re all taking safety precautions.
At Cleveland Clinic, for example, those precautions include:
If someone is having a heart attack or stroke, being treated quickly can improve their chances of recovery.
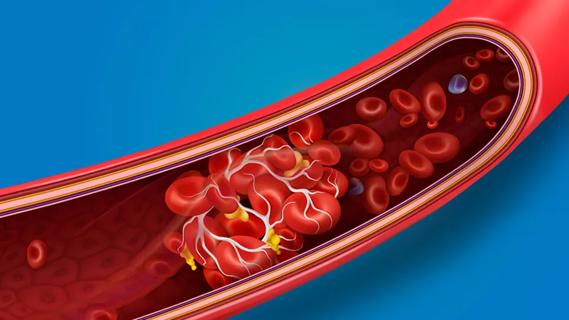
A stroke happens when brain arteries rupture or when a blood clot cuts of blood supply to part of the brain. Life-saving medicine called recombinant tissue plasminogen activator (tPA) needs to be given within 4 ½ hours after symptoms start. Specialists can also perform emergency procedures to remove a clot or control bleeding, but these, too, must be done quickly.
The longer the brain goes without fresh blood and oxygen, the more brain cells die – and that damage is irreversible.
The same is true for a heart attack. “When you wait to get treatment, the heart muscle dies, and when it dies, then your heart doesn’t have the necessary pumping capabilities that it needs,” Dr. Borden says.
Anyone who is experiencing symptoms of a stroke, heart attack or another medical emergency should call 911 right away. These include:
Advertisement
Remember, whether COVID-19 or a health emergency, it’s always best to promptly seek the care you need. So don’t delay!
Advertisement
Learn more about our editorial process.
Advertisement

The medication is ineffective and — in the case of animal ivermectin — potentially dangerous

Updated vaccinations are recommended to better protect against the evolving virus

Enteroviruses are often to blame for summer colds, leading to a runny nose, sore throat and digestive symptoms

Redness, swelling, itching and rash can happen when your body’s immune system reacts to the vaccine injection

Studies suggest 1 in 5 people infected with the coronavirus never develop symptoms
An increased risk of blood clots can last for nearly a year after a COVID-19 diagnosis

COVID-19 may be associated with tinnitus, but research is still ongoing

The short answer: It’s complicated, but the basic care precautions still prevail, like washing your hands and isolating if you’re sick

Focus on your body’s metabolic set point by eating healthy foods, making exercise a part of your routine and reducing stress

PFAS chemicals may make life easier — but they aren’t always so easy on the human body

While there’s little risk in trying this hair care treatment, there isn’t much science to back up the claims