Advertisement
Get the facts before assuming the worst

If you’re living with some type of allergy, you’re already on high alert daily to prevent allergic reactions. So, when you hear that some people have experienced allergic reactions after receiving COVID-19 vaccines, you might be wondering if you should get the shot.
Advertisement
Cleveland Clinic is a non-profit academic medical center. Advertising on our site helps support our mission. We do not endorse non-Cleveland Clinic products or services. Policy
David M. Lang, MD, allergist and Chair of Cleveland Clinic’s Department of Allergy and Clinical Immunology, has a few reasons why you shouldn’t hesitate to get vaccinated against COVID-19.
Between December 14-23, 2020, monitoring by the Vaccine Adverse Event Reporting System detected 21 cases of anaphylaxis after 1,893,360 first doses of the Pfizer-BioNTech COVID-19 vaccine. This evened out to about 11.1 cases per million doses. Seventy-one percent of these cases also occurred within 15 minutes of vaccination.
Since then, the Centers for Disease Control and Prevention (CDC) has stated that anaphylaxis after COVID-19 vaccination is rare. In the U.S., about two to five people per million vaccinated have experienced anaphylaxis so far. But this isn’t exclusive to COVID vaccines. Severe allergic reactions can occur after any vaccination.
“Even though there is a risk of anaphylaxis, it’s still very small — and the potential benefit from the COVID-19 vaccination clearly exceeds the potential for harm,” says Dr. Lang. “The situation is evolving, however, and we’ll learn more as we continue to work with these vaccines.”
It’s recommended that if you’ve had an allergic reaction to any of the ingredients in the available vaccines, talk to your healthcare provider first. For instance, if you’ve had an allergic reaction to an ingredient in one of the mRNA vaccines (Moderna and Pfizer-BioNTech), your provider might suggest Johnson & Johnson’s COVID-19 vaccine. Or, if you’re allergic to any ingredient in Johnson & Johnson’s COVID-19 vaccine, your provider might recommend an mRNA vaccine. This can also apply if you had an allergic reaction to the first dose of a COVID-19 vaccine.
But having seasonal allergies or a shellfish allergy doesn’t mean that you can’t get vaccinated.
Here’s a breakdown of what’s in the three COVID-19 vaccines that have either been FDA-approved or approved for emergency use.
According to Pfizer, the Pfizer BioNTech COVID-19 vaccine is a messenger RNA (mRNA) vaccine that was made with synthetic and chemically produced components as well as enzymatically produced components from naturally occurring substances like proteins. This vaccine does not have a live virus in it.
Inactive ingredients in the Pfizer BioNTech COVID-19 vaccine include:
Moderna’s vaccine is similar to Pfizer BioNTech’s and also has no live virus in it. Its ingredients include:
Unlike the other vaccines, the Johnson & Johnson vaccine is a single-dose viral vector vaccine, which uses an adenovirus (the kind of virus that typically causes colds) to harmlessly deliver the DNA code into your cells. Besides those virus particles, the ingredients of this vaccine include:
Advertisement
“It’s believed that COVID-19 vaccine-related allergic reactions are caused by polyethylene glycol (PEG), an ingredient in the vaccines,” says Dr. Lang. “Whether some of the reactions are occurring via another mechanism is unclear at this time.”
While hearing about allergic reactions to COVID-19 vaccines can be worrisome, Dr. Lang believes educating patients about the infrequency of adverse reactions and breaking down common vaccination myths can help put more people at ease.
“Many times, patients claim they got sick from a vaccine when they’re really referring to a natural immune response from the vaccine. Fever, chills and muscle aches can occur within 36 hours of vaccination because a patient’s immune system is responding appropriately in developing immunity after receiving the vaccine. It’s not an allergic reaction.”
He adds that delayed reactions due to immune response, as well as fatigue, soreness at the injection site and vasovagal reactions(drop in blood pressure, fainting episodes), are not cause for avoiding COVID-19 vaccines. This is especially important to keep in mind if a reaction occurs after the first dose of a two-dose COVID-19 vaccination regimen.
If you’ve had a severe allergic reaction to another vaccine or injectable medication — or have experienced anaphylaxis from any cause — you can still receive the COVID-19 vaccine. However, your vaccination should be followed by a 30-minute observation period in a setting where personnel, equipment and supplies are present to manage anaphylaxis.
Advertisement
“Anaphylaxis commonly occurs within 30 minutes of exposure and would be unusual after 60 minutes,” says Dr. Lang.
Patients with allergies to other medications, foods or inhalants can receive the COVID-19 vaccine with normal precautions. This typically includes a 15-minute observation period after the injection based on CDC guidelines.
While about 10% of the population has reported a penicillin allergy, less than 1 in 10 of those people are truly allergic. About 80% of those who were once allergic to penicillin lose their sensitivity to it after 10 years. Dr. Lang says that you can still get vaccinated even if you’re allergic to penicillin. Since December of 2020, more than 390 million doses of COVID-19 vaccines have been given in the United States. And the CDC says the vaccines are safe and effective. If you’re not sure about what you should do, talk to your provider.
It’s not recommended to take pain relievers or allergy medications before you receive a COVID-19 vaccine. Doing so could interfere with the body’s immune response to the vaccine. So if you’re thinking about taking allergy medicine before your appointment, Dr. Lang says it’s not necessary.
Advertisement
Learn more about our editorial process.
Advertisement

Most routine vaccines are safe for people living with multiple sclerosis — but be sure to talk with your care team about your needs

The medication is ineffective and — in the case of animal ivermectin — potentially dangerous

Updated vaccinations are recommended to better protect against the evolving virus

Enteroviruses are often to blame for summer colds, leading to a runny nose, sore throat and digestive symptoms

Redness, swelling, itching and rash can happen when your body’s immune system reacts to the vaccine injection

Studies suggest 1 in 5 people infected with the coronavirus never develop symptoms
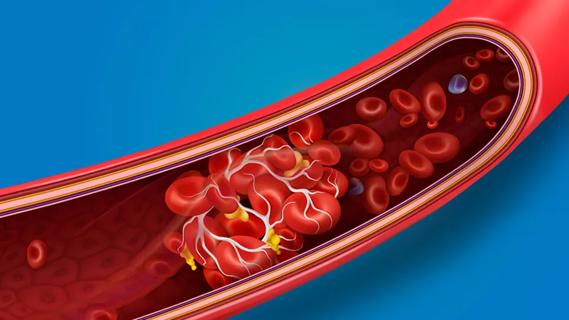
An increased risk of blood clots can last for nearly a year after a COVID-19 diagnosis

The answer varies from person to person and vaccine to vaccine

Focus on your body’s metabolic set point by eating healthy foods, making exercise a part of your routine and reducing stress

PFAS chemicals may make life easier — but they aren’t always so easy on the human body

While there’s little risk in trying this hair care treatment, there isn’t much science to back up the claims